A phase II test found that T-VEC improved tumor detection in 50% of patients, leading to an early study, with strong immunocomic activation and minimal side effects.
Study: Effectiveness and tolerance of Talimogene Laherparepvec Treatment in Neo -Dependent Treatment. Credit Picture: Kateryna Kon/Shutterstock.com
In a recent study published in Cancer natureResearchers evaluated the tolerance and efficacy of a new active onocytic therapy (OV) in skin cell carcinoma (BCC).
Background
The incidence of BCC skin, the most common cancer worldwide, has doubled over the last 20 years and is expected to increase further. Treatment for most BCCs is surgical resection, which has a risk of recurrence up to 15%.
Based on the size and detection of the BCC, plastic reconstructive surgery could be required, which can complicate the detection of early local relapse and therefore adversely affect the quality of life and well -being of patients.
In locally advanced and difficult to detect BCCs, Neoadjuvant’s therapeutic approaches aim to reduce post-surgical morbidity, increase the chances of therapeutic resection and relieve the risk of recurrence.
Treatment with neovascular hedgehog inhibitors has a total of 71%response rate (ORR), but side effects (AEs) such as fatigue, muscle cramps, hair dysfunction and hair loss often lead to interruption and low compliance.
OVS represents an intra-therapeutic therapeutic category that can be a safe and effective treatment of neo-vascular therapy for BCCs of difficult resolution.
Talimogene Laherparepvec (T-VEC) is an OV, a genetically modified herpes simplex virus (HSV1), approved for the treatment of injectable, irreversible melanoma lesions in the United States and Europe. The T-VEC has a dual way of action and can change the tumor microenvironment (TME) by activating adaptive and innate immunity.
The study and findings
The present study presented the results of a Phase II clinical test of T-VEC, two-stage, two-stage, skin BCCs. The group participated in 18 patients aged 49-92 from January 2020 to January 2022 and assigned them to the treatment with Neoadjuvant T-VEC.
The main point was the percentage of subjects who, during surgery after six T-VEC cycles, became detectable with the closure without the need for plastic reconstructive surgery.
Nine patients showed a positive primary endpoint. Orr was 55.6%. Six patients achieved complete response (CR), four had partial response and eight had a stable disease. The size of the tumor was not increased in any patient throughout treatment.
Twelve patients achieved pathological non-CR (non-PCR) and six had a pathological CR (PCR). The average decrease in the tumor area was 45.4% until surgery.
Patients with positive and negative primary endpoints had an average decrease in the tumor area of 62.5% and 37.7% respectively. The rates without relapse and the total survival rates were 100% in six months. However, in an average 11 -month follow -up, two patients developed new BCCs.
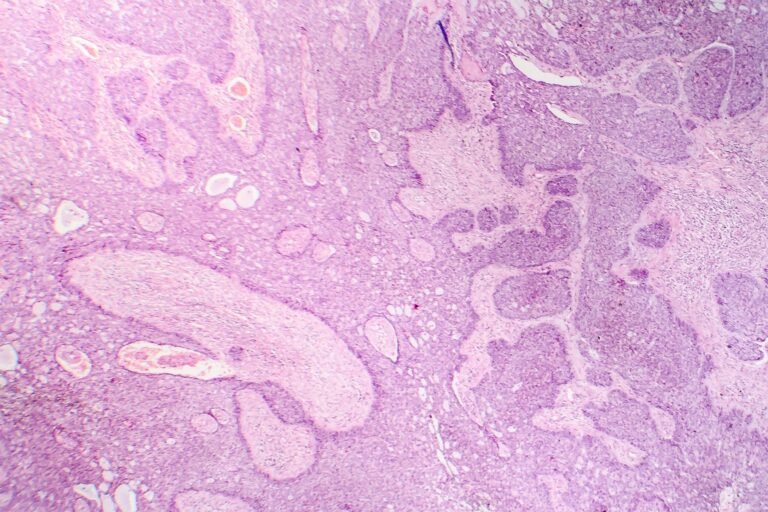
Four patients had AE-related AEs. No serious SA happened. Further, the spatial profile was performed with multiple treatment with immunofluorescence staining before and after T-VEC.
This analysis revealed a significant increase in diversification cluster 8+ (CD8+) T cells, CD68+ myeloid cells and CD20+ B cells and decrease in CD4+ T controller (tcan) Cells and CD4+ T cells after treatment with T-VEC.
In addition, there was a significant increase in CD8+ T cells, CD68+ myeloid cells and CD20+ B cells that penetrate the interconnection of the islands of the tumor after treatment, with a significant decrease in the density of tumor cells in patients with remaining tumor after treatment.
T-cells were a significant proportion of immune cells in the TEM. Further analyzes revealed eight clusters of cells and a cluster of natural killer cells after treatment.
Topics with non -PCR showed higher tcan Cells, while those with PCR had significantly increased cytotoxic T cells in-tcan Cell ratio. Additional experiments revealed small, large, medium and over-expanded cell clones T.
Cytotoxic T cells were the majority of the over-expanded cell clones. There was a significant increase in CD68+ Macrophages after treatment with T-VEC.
Analysis of a RNA cell (SCRNA-SEQ) revealed further separate myeloid cell populations after treatment. Ficolin 1- and the C1Q C-Positive Macropharian supplement were the majority.
Analyzes of B cell subsets showed nine clusters of plasma and B cells, with heterogeneity intra-and between patients. The sequence of integrated SCRNA-SEQ sequence and a single cell cell (BCR) revealed that half of the BCR repertoire included over-expanded or large clones.
Only plasma cells showed over-extension, while B cells showed small and medium extension. The over-exported plasma cell clones were almost exclusively immunoglobulin heavy constant C 1 (IGHG1)-positive.
Conclusions
The findings show that the treatment with neo-energy T-VEC was well tolerated and could reduce the size of the BCC tumor, simplify surgery and lead to a complete pathological recession.
In addition, T-VEC treatment significantly changed the intra-abdominal synthesis of immunocytes and caused strong immune response.
In addition, over-expanded IGHG1 Plasma cells and cytotoxic T cells were detected. Overall, these results are promoted by OVs as a therapeutic strategy for skin BCCs.