Feeling anxiety before surgery is normal – but for many patients, it goes far beyond the nerves. There is one growing body of research By showing that poor mental health before surgery can derail recovery in ways that extend far beyond surgery.
For example, in recent surveyMy colleagues and I have found that stress and depressive symptoms before surgery are linked to poorer surgical results. This includes higher rates of complications within 30 days and even an increased risk of death within one year.
In addition, many patients classify stress as one of worst parts of their surgical experienceworse than pain or other aspects of surgical recovery.
Both patients and clinical doctors Identify the need to support mental healthBut this need is often overlooked. As an expert in perioperative mental health, I have some solutions to offer.
Demand for surgery is accelerating
The increasing number of surgical patients-driven by aging population, increasing rhythms of chronic diseases and developments in medicine-has intensified the pressure on the healthcare system.
The growing demand has led to longer waiting times and Increases in surgery delays and cancellations. This situation has become even worse than the Covid-19 pandemic. Patients can remain pain in the vacuum for weeks, months or even years.
My colleagues and I found These delays of surgery and cancellations must be linked to even further negative effects on mental and physical health. Patients get worse while waiting.
While this growing delay represents a major challenge, it also presents an opportunity.
The opportunity
The surgical waiting period, which is very often prolonged, offers a critical window to detect patients with a higher risk for poor mental health. Determination of those in need is critical to providing targeted and scientifically supported psychological therapies. It is a time when patients have already been involved in the healthcare system, they are motivated to do good and receptive to guidance.
Psychological treatments based on evidence such as cognitive behavioral treatment before surgery have been shown to improve results such as pain and function.
International Organizations, such as World Health OrganizationThey emphasize the importance of including mental health support in hospital environments, including surgical care.
In the United States, the Center for perioperative mental healthcoming from the University of Washington, is one of the Large -scale first initiatives of its kind with the aim of integrating personalized paths to support mental health for elderly adults.
As an external counseling chair for this center, I have seen how initiatives such as they can significantly enhance perioperative care and patient results.
At the global level, efforts such as programs before construction-which are aimed at enhancing surgical readiness through exercise, nutrition and mental health support-are recording. While they represent progress, they are not systematically applied, often not integrating mental health care based on evidence and evidence and Show mixed results Because of the variability of design and tradition.
There are powerful elements that associate poor preoperative mental health with the worst results, along with the clear demand of patients and the promising results from existing programs. However, Regional Mental Health Support in Canada remains subjective and far from standard clinical care.
Mental health is still non -repaired in surgical facilities.
Canadian type/ryan remiorz
Utilize technological developments
Given the important Mental Health Accessible Care Jobs in CanadaCreative solutions are critical. One way forward is to make the most of the rapidly growing technology.
For example, our team has developed a Program Innovative Virtual Reality (VR) Using patients input and strategies supported by science in Mental Health Support before Surgery.
Patients found it both acceptable and useful. These platforms help patients They are mentally prepared for surgery, familiarize with the environment and feel more in control.
Other large -scale digital initiatives such as Power of Power over Pain Offer free psychological therapies for managing pain from the comfort of your home. And pain management is especially important for those who expect extensive periods for many types of surgery.
Our multi -scientific team at the University of Manitoba believes that these types of digital approaches can be delivered on a scale, relatively low cost and with high acceptance and satisfaction of patients. This is not meant to replace human care, but to expand it.
These are not only fancy gadgets but clinical tools with a real possibility of integrating mental health therapies based on evidence.
Prepare physically and mentally
Healthcare systems are often not sufficient and Canada is no exception. To deal with this, surgical care should prioritize greater investment in mental health support, including the integration of technology. These efforts can better prepare patients physically and mentally for surgery and help in their surgical recovery.
(National Cancer Institute/Unsplash); Cc by
Mental health is central to surgical results – not secondary. We need a national strategy to finance research and ultimately implement ordinary accessible mental health treatments for surgical patients. This is especially important for those who have a higher risk.
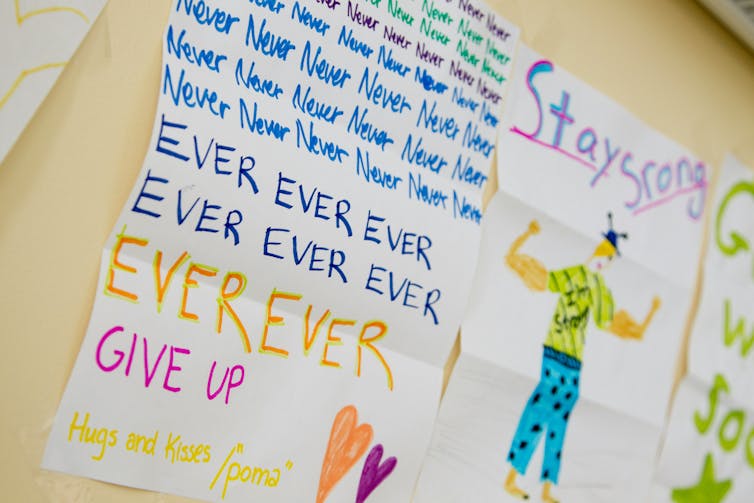
Our patients have told us what they need. The evidence is undoubtedly. And the opportunity to change was never bigger. We need to build a system that really cares for the whole patient.
