A new AI tool reads lung cancer slides in less than an hour, predicting accurate mutations and storing patients’ delays, cost and tissue loss, signaling a turning point in precision cancer care.
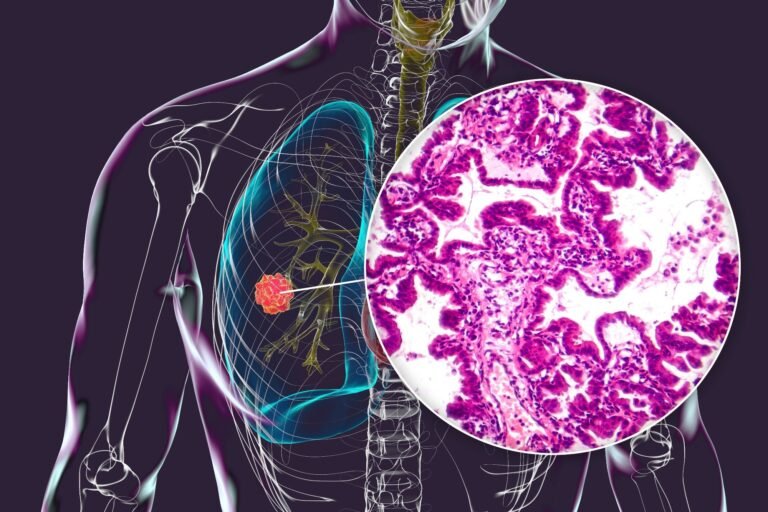
Study: Real Development of a Pathology Foundation Model for the Real World for Detecting Biomarkers of Lung Cancer. Credit Picture: Kateryna Kon/Shutterstock.com
A recent Natural medicine The study has compiled a large international clinical set of digital pulmonary adenocarcinoma (LUAD) to facilitate the development of a computing epidermal growth factor (EGFR).
Tests for EGFR mutations in adenocarcinoma of the lungs
Luad is the most common form of lung cancer, with EGFR being the most common physical mutation in kinase genes. Exact EGFR tests are vital to ensure that patients receive the right first -line treatment. The EGFR test is done for patients with advanced stages. Otherwise, molecular tests in lung cancer are the standard research line. EGFR tests are significantly lower than the level determined by clearly published instructions. There could be many reasons, including technical obstacles in acquiring and processing samples for testing and inadequate material from diagnostic biopsies.
Computing methods for detecting EGFR mutations can significantly improve the clinical work flow for diagnostic biopsies of lung cancer. Only digitized pathology slides from diagnostic hematoxylin and eosin (H & E) will be used as a substrate, allowing the result to be reported without physical treatment and minimal costs. Immediate production of results should also allow all other decisions to be updated.
For the study
This study developed the eagle (EGFR AI Genomal Evaluation of the Lungs) and presented its clinical utility as a computing biomarker based on H&E. The aim was to enhance the standard molecular work flow using the diagnostic biopsies of Luad patients. Unlike traditional workflow, AI sorting often excludes rapid tests. This was done when maintaining the overall high sorting performance. Next -generation sequence tests (NGS) are still required for samples that have been positively examined.
A large international clinical set of digital pulmonary adenocarcinoma (Luad) was drawn up to train the algorithm according to the broad biological and technical volatility expected by real clinical development. A total of 5,174 slides from Memorial Sloan Kettering Cancer Center (MSKCC) were used to refine a state -of -the -art foundation model. The model was validated using 1,742 internal slides from MSKCC and in external test groups to ensure health.
These included institutions in the United States and Europe and covered multiple slide scanners, demonstrating the generalization of the model in institutions and multiple scanners. A silent test was carried out with the development of the eagle in real time to simulate its performance in a real environment.
Study findings
Eagle took place at the expected level in new cases and was considered suitable for clinical application. The results of the EGFR rapid test were compared to the results of the IdyLla test. Idylla showed a positive prognostic value (PPV) 0.988, sensitivity of 0.918, 0.993 specialization and negative prediction (NPV) 0.954 during the analyzed period. The model achieved an area below the curve price (AUC) 0.847. The performance was less accurate in metastatic samples (AUC 0.75) compared to primary samples (AUC 0.90).
Using the amount of tissue as a proxy for the amount of volume, the surface was calculated on the basis of the tiles used for model conclusions. There was a general trend in which the performance of the model was enhanced as the area of analyzed tissue increased. Further tests have revealed that the model was able to detect all clinical related EGFR mutations, thus pointing out the strength of the eagle between variants. The performance of the model to external groups was also in accordance with internal validation and showed AUC 0.870.
A silent test was conducted on MSKCC to test the actual application. As in the previous case, the performance of the model was lower in metastatic samples (AUC 0.760), compared to primary samples (AUC 0.896). Lymph nodes (AUC 0.74) and bones (AUC 0.71) performed particularly bad. The total AUC was comparable to the previous results at 0.853. These results further supported the development of the eagle for primary samples. Artificial artificial intelligence work (AI) could lead to a lower number of samples tested rapidly, based on eagle exit.
Three threshold strategies were investigated in the test to determine how many rapid tests could be saved while maintaining performance comparable to traditional work flows. Depending on the chosen threshold, the work flow resulted from AI reduced rapid tests by 18% to 43%, while maintaining high NPV and PPV values.
The recovery time for Eagle was also a key advantage, providing results in just 44 minutes, significantly faster than the few 48 hours required for rapid tests and several weeks for NGS.
The actual setting of the silent test was important, as it helped researchers understand how the recently invented protocol was performed, including possible sources of false negative and false positive results. By examining the thermal maps of attention overlapping tissue slides, the group acknowledged that the false positives often included biologically related mutations such as ERBB2 or Met Exon 14 imports bypassing the events. False negatives tend to appear in samples with minimal tumor architecture, such as samples of cytology or heavy blood biopsies.
It is assumed that the error rate could be significantly reduced if physicians manually interpret the results. The eagle is not intended to replace the NGS sequence, but it is only a sorting test. Eagle is intended to identify potential positive cases and effectively exclude EGFR mutations. Because Eagle does not distinguish between EGFR subtypes that require different targeted treatments, NGS confirmation is still necessary before choosing treatment.
Conclusions
This study presented a validated computational pathology model for the detection of EGFR mutation in Luad. The model can reduce tissue consumption, improve diagnostic efficacy and accelerate Ai’s adoption in clinical practice. Eagle achieved his performance by perfecting a model of vision transformers, emphasizing a shift to the most generalized AI tools in pathology. Future research should examine additional biomarkers and study them in a prospective clinical trial.
Magazine report:
- Campanella, G., Kumar, N., Nanda, S. et al (2025). The actual development of a pathology foundation model for the detection of biomarkers of lung cancer. Natural medicine. Doi: https://doi.org/10.1038/S41591-025-03780-X. https://www.nature.com/articles/S41591-025-03780-X