Background and Significance
Sexual and mental health are deeply intertwined.
Post-SSRI sexual dysfunction (PSSD) is a type of sexual dysfunction associated with commonly prescribed antidepressants, including selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and certain tricyclic antidepressants. PSSD is distinct from depression-related sexual dysfunction. Genital numbness, also known as post-treatment persistent genital hypoesthesia (PPTGH) is a common symptom of PSSD.
PSSD is a largely unknown disorder due to a lack of research and awareness. It is important that sexual health practitioners know about PSSD so they can support people who may seek help or describe symptoms of PSSD.
Patients usually report reduced genital sensitivity or numbness in the genital area. However, in these cases the numbness does not go away, even after stopping the long-term antidepressant. Research has found that some people who experience PSSD have permanent damage to the erectile tissue found in the nipples, penis and clitoris.
In 2021, Health Canada issued a safety report warning that SSRIs and SNRIs may cause long-term sexual dysfunction that may persist after medication is discontinued, and that persistent sexual side effects of antidepressants are likely to be underreported.
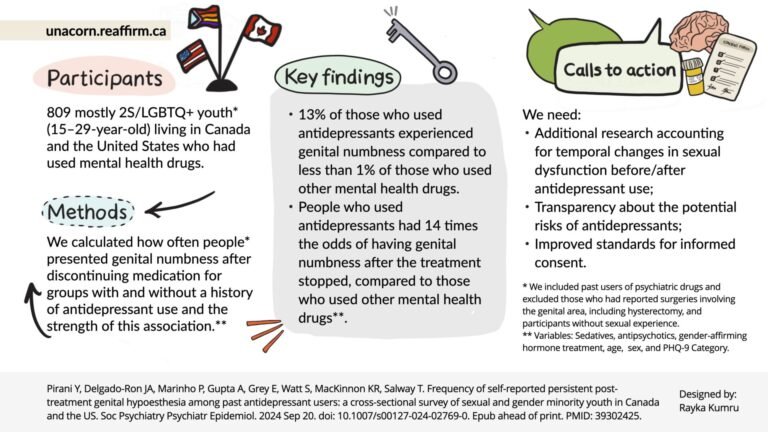
A team of researchers at Simon Fraser University asked about PSSD symptoms in a general survey of sexual and gender minority youth.
Summary of evidence
A total of 2179 subjects with a history of psychiatric treatment participated in this study. We excluded sexually naïve subjects who had undergone genital surgery and controlled for factors such as hormone therapy, age, and sex. Among those who had discontinued treatment, 13% of former antidepressant users (93/707) reported persistent genital numbness compared with 1% (1/102) among former users of another psychiatric medication. We found that former antidepressant users were 14 times more likely to report persistent genital numbness compared to the other group (OR: 14.2, 95% CI: 2.92 to 257).

Implications for practice
PSSD can be a debilitating and emotionally devastating condition. It can seriously affect a person’s quality of life, mental health and has been a factor in suicide for some. PSSD may begin as soon as the person starts taking antidepressant medication, or it may not become apparent until after discontinuation. Some cases of PSSD resolve over time – however many persist indefinitely. There is no known cure for PSSD.
Our key recommendations include that:
- Policy makers include information about PSSD in the product monograph of antidepressants.
- Clinicians should engage in discussions about potential complications before initiating treatment.
- Research is needed to better understand the prevalence and symptoms of PSSD to provide evidence-based guidance.
People often enter treatment without any knowledge about the possibility and long-term effects of PSSD. Clinicians should support people in making an informed decision before starting treatment. Prescribers should also assess sexual function and symptoms before, during, and after treatment.
PSSD is often overlooked or misdiagnosed. When symptoms are misattributed to psychological causes, this can create further alienation. Clinicians can validate patients’ experiences to prevent feelings of shame and self-blame.
Other sexual symptoms of PSSD can be seen here. Nonsexual symptoms of PSSD are related to emotional numbing, cognitive impairment, depersonalization, and other sensory problems.
In 2022, diagnostic criteria were published that can be used by clinicians to establish a diagnosis (see resources below). Currently, there is limited support available for people experiencing PSSD. Sexual health physicians can play a key role in supporting meaningful support in the health care system.


For more information
Pirani Y, Delgado-Ron JA, Marinho P, Gupta A, Gray E, Watt S, MacKinnon KR, Salway T. Prevalence of self-reported persistent genital hypoesthesia after treatment among former antidepressant users: a cross-sectional survey of sexual and gender minority youth in Canada and the USA. Soc Psychiatry Psychiatr Epidemiol. 2024 Sep 20. doi: 10.1007/s00127-024-02769-0. Epub ahead of print. PMID: 39302425.
Antidepressant Use and Genital Numbness Among Sexual and Gender Minority Youth – A Health Care Resource
Antidepressants & Genital Numbness – source
RxIsk – RxISK: Making medicines safer for us all
PSSD Canada – Canadian PSSD Society
PSSD network – The PSSD Network
Sidefxhub – Organization of PSSD & PFS patients
References
Bolton JM, Sareen J, Reiss JP. Genital anesthesia persists six years after discontinuation of sertraline. J Sex Mart Ther. 2006? 32 (4): 327-30.
Canada Vigilance Program. (2021). Adverse reaction number 000925645. See here: hips://www.pssdcanada.ca/new-page-77
Search Health Canada’s Adverse Drug Database: hips://www.- canada.ca/en/health-canada/services/drugs-health-products/medeffect- canada/adverse-reac-on-database.html
Clayton AH, Croft HA, Handiwala L. Antidepressants and sexual dysfunction: mechanisms and clinical implications. Postgrad Med. 2014 Mar;126(2):91-9. doi: 10.3810/pgm.2014.03.2744. PMID: 24685972..
Chinchilla Alfaro, K., van Hunsel, F., & Ekhart, C. (2022). Persistent sexual dysfunction after SSRI withdrawal: A review of the scope and presentation of 86 cases from the Netherlands. Expert Opinion on Drug Safety, 21(4), 553-561. 10.1080/14740338.2022.2007883
Healy D, Bahrick A, Bak M, Barbato A, Calabrò RS, Chubak BM, et al. Diagnostic criteria for persistence of sexual dysfunction after treatment with antidepressants, finasteride and isotretinoin. Int J Risk Saf Med. 2022? 33 (1): 65-76.
Healy D, Le Noury J, Mangin D. Sexual dysfunction after SSRI: Patient experiences of engagement with health professionals. International Journal of Risk and Safety in Medicine. 2019? 30:167-178.
Healy, D. (2018). Citizen Petition: Sexual side effects of SSRIs and SNRIs. International Journal of Risk and Safety in Medicine, 29(3-4), 135-147. Retrieved from: hips://www.ncbi.nlm.nih.gov/pmc/ar-cles/PMC6004927/
Healy, D., Le Noury, J, & Mangin, D. (2018). Persistence of sexual dysfunction after treatment with antidepressants, 5α-reductase inhibitors and isotretinoin: 300 cases. International Journal of Risk and Safety in Medicine 29(3-4), 125-134. Retrieved from: hips://pubmed.ncbi.nlm.nih.gov/ 29733030/
Health Canada. Summary Safety Review – Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs). reg-content/summary-safety-review-detail.php?lang=en&linkID=SSR00254
Hogan C, Le Noury J, Healy D, Mangin D. One hundred and twenty cases of persistent sexual dysfunction after treatment. Int J Risk Saf Med. 2014? 26 (2): 109-16.
Pirani Y, Delgado-Ron JA, Marinho P, Gupta A, Gray E, Watt S, MacKinnon KR, Salway T. Incidence of self-reported persistent genital hypoesthesia after treatment among former antidepressant users: a cross-sectional survey of sexual and gender minority youth in Canada and the USA. Soc Psychiatry Psychiatr Epidemiol. 2024 Sep 20. doi: 10.1007/s00127-024-02769-0.
Reisman Y. Post-SSRI sexual dysfunction. British Medical Journal. 2020? 368: m754. PMID 32107204.