As anyone who has ever tried to navigate health care coverage can attest, it is too often a frustrating, fruitless endeavor marked by multiple phone calls, numerous transfers, and invariably long wait times. This cumbersome process creates a barrier for those seeking medical care and can disproportionately affect transgender individuals seeking treatment for gender dysphoria.
A transgender person is a person whose gender does not align with the gender they were assigned at birth. This discrepancy between gender and gender identity can cause significant psychological distress in a transgender person, which is known as gender dysphoria.
Gender dysphoria can lead to feelings of worry, anxiety and depression. The certainty that one’s true gender is not reflected by one’s body can be an extremely painful experience that affects all areas of a person’s life. Transgender people may feel disgusted by their genitalia and other sex-related physical characteristics and have a strong desire to get rid of them. This chronic state of anxiety can lead to thoughts or actions of self-harm or even suicide. A 2015 national survey of transgender people found that 40% of survey respondents had attempted suicide at least once in their lifetime, with 7% having attempted suicide in the past year.
To compound matters, transgender people face a higher rate of health disparities than the average US citizen. The aforementioned 2015 survey revealed that 29% of transgender respondents lived in poverty, and more than half (55%) of those surveyed had been denied coverage for transition-related surgery, while a quarter had been denied coverage for transition- related hormone therapy.
With this information in mind, the authors of a 2020 Journal of Sexual Medicine The study aimed to determine which US Medicaid programs cover gender-affirming hormone therapy (GAHT) and which cover gender-affirming surgery (GAS) for transgender people. GAHT and GAS, along with counseling to support transgender people in their transition are the three dominant health services for gender dysphoria at the moment.
The results showed that GAHT and GAS are not covered by all state Medicaid programs, and although many states’ Medicaid programs cover these treatments, information was often difficult to find, requiring several phone calls and considerable time to locate.
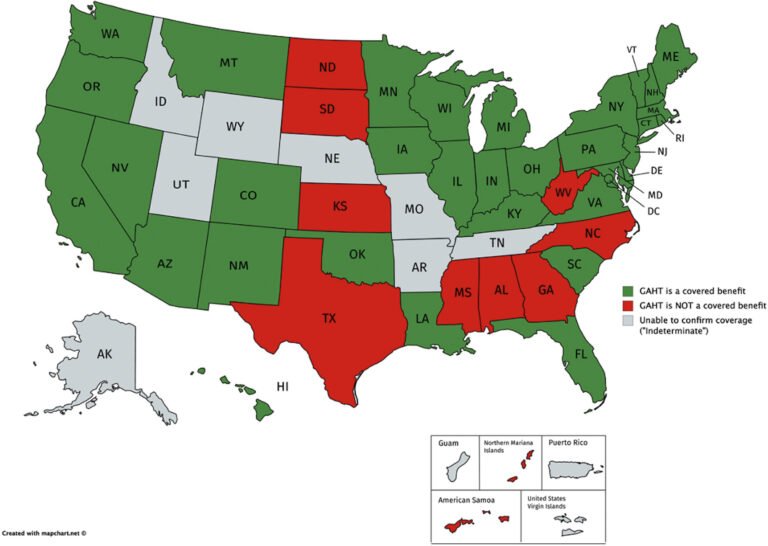
According to this study, GAHT is covered by 34 of 51 state Medicaid plans (including Washington, DC), not covered by 9 of 51 state plans, and coverage status was deemed “undetermined” in 8 of 51 states (Figure 1). To find this information, the authors completed an average of 3 phone calls per state (range 1-10 phone calls) and spent an average of 31.8 minutes on the phone for each unique call (range 1.5-124.8 minutes).
GAS is even less likely to be covered by Medicaid than GAHT, and is covered by only 25 of the 51 state Medicaid programs. Not covered by 22 of 51 state programs, and coverage was classified as “undetermined” in 4 of 51 states (Figure 2). Researchers completed an average of 3.3 phone calls per state to obtain this information (range 1–12 phone calls) and spent an average of 33.2 minutes on the phone during each call (range 1.5–119 .8 minutes).
The authors of this study concluded that there are many barriers to accessing health care for transgender people, and that the process of determining coverage for medical treatments can be very challenging and time-consuming for these patients.
Figure 1. Maps of all 51 US states (including the District of Columbia) and 5 US territories, colored by whether GAHT is a covered benefit (green), not a covered benefit (red), or if coverage remains “undetermined” (gray). This image was published by The Journal of Sexual Medicine, 18(2), Zaliznyak, M., Jung, EE, Bresee, C., & Garcia, MM, Which US Medicaid Programs? do they provide coverage for gender-affirming hormone therapy and gender-affirming surgery for transgender patients? -State-by-state review and a study detailing patient experience to confirm coverage of services, p. 415, Copyright Elsevier (2021).
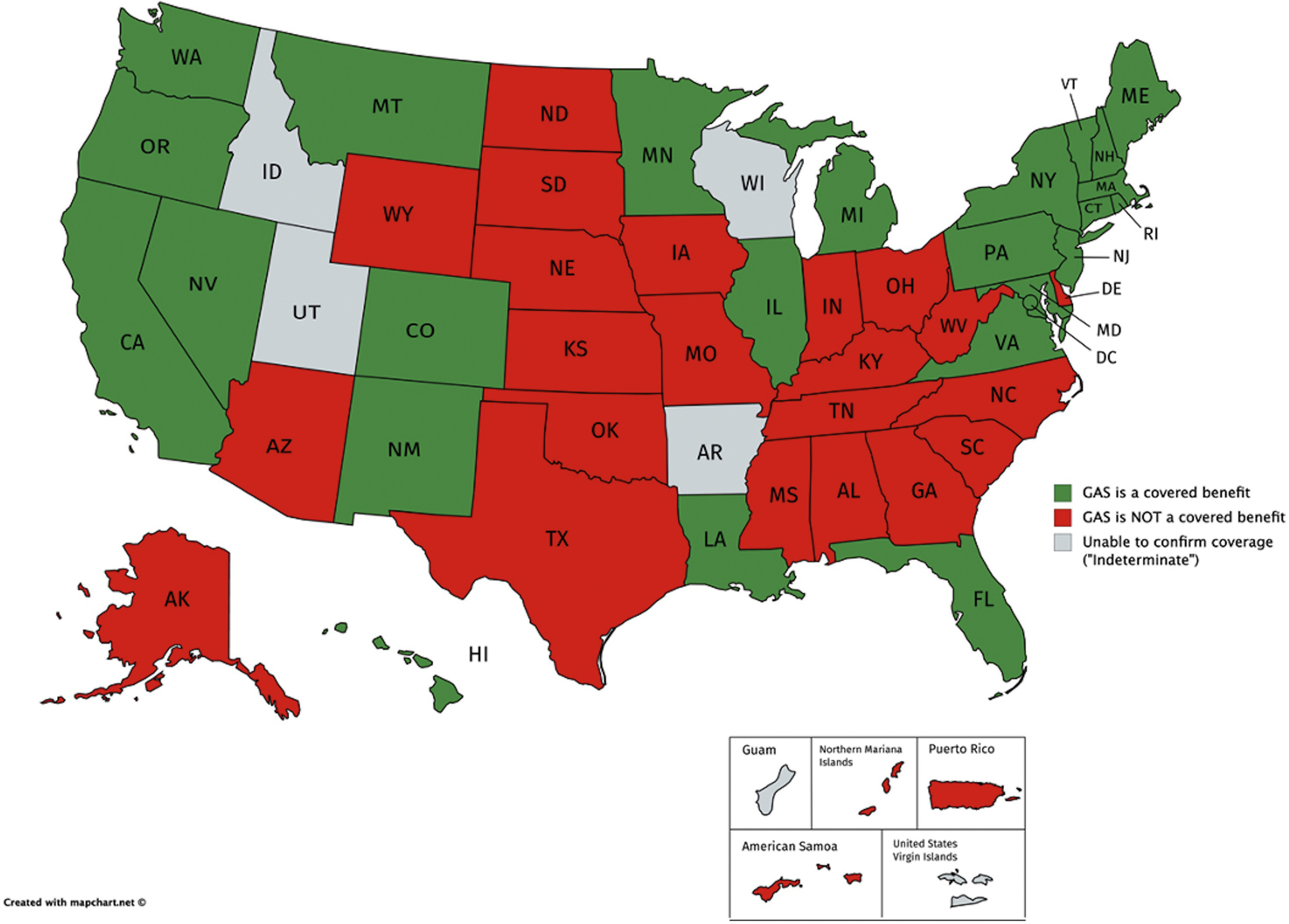
Figure 2. Maps of all 51 US states (including the District of Columbia) and 5 US territories, colored by whether GAS is a covered benefit (green), not a covered benefit (red), or if coverage remains “undetermined” (gray). This image was published by The Journal of Sexual Medicine, 18(2), Zaliznyak, M., Jung, EE, Bresee, C., & Garcia, MM, Which US Medicaid Programs? do they provide coverage for gender-affirming hormone therapy and gender-affirming surgery for transgender patients? -State-by-state review and a study detailing patient experience to confirm coverage of services, p. 416, Copyright Elsevier (2021).
Resources:
Zaliznyak, M., Jung, EE, Bresee, C., & Garcia, MM (2021). Which US Medicaid Programs do they provide coverage for gender confirmation hormone therapy and genital surgery for transgender patients?: A state-by-state review and study detailing the patient experience of confirming coverage of services. The Journal of Sexual Medicine, 18(2), 410-422.