Esophageal adenocarcinoma (EAC), one of the two large forms of esophageal cancer, is the sixth most deadly cancer worldwide for which there is no effective targeted treatment. Patients should be based on chemotherapy as a model of care, which begins prior to surgery as a so -called “neo -active chemotherapy” in the hope of shrinking or controlling tumors. However, most patients become resistant to some Nacts, leading to bad results.
Given the absolute lack of therapeutic alternatives, correspondents and non -respondents continue to receive one of the available chemotherapy without knowing whether it will work. Even in correspondents, chemotherapy of the choice may not completely stop their tumors from moving and transformed and may have toxic side effects on the body. The availability of a personalized oncological precision model that can accurately predict the response of a patient to different Nacts in time is a critical unfulfilled need.
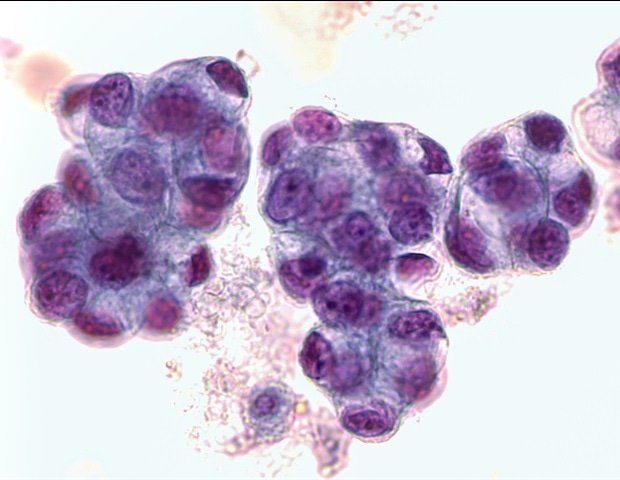
The researchers had developed the so-called “organoids” of EAC biofuid cells, which are 3D esophageal mini-organs formed by specifically for stem cell tissues that have critical characteristics of the esophageal epithelial lining. However, they do not have significant ingredients of this particular microevalbal tumor of a patient (TME), such as stomatic fibroblasts and collagen fibers and therefore do not show the same responses to Nact as real tumors.
Now, a research collaboration led by Donald Ingber, MD, Ph.D., Founding Director at the Wyss University Institute of Biological Inspired Engineering at Harvard University and Lorenzo Ferri, MD, who is head of the thoracic division of the thoracic and higher gastrointestinal. Montreal, it has promoted a personal medicine solution with the ability to improve chemotherapy patients.
The researchers have utilized the Wyss Institute’s microfiber technology of the Wyss Institute and used it to co-cultivate EAC organoids next to layer cells isolated from the same biopsies received by the McGill group from EAC patients in a clinical study of coin. With the recapitalization of some of the inherent TME complexity in vitroThe group was able to predict the reactions of patient tumors to the NACT standard much more accurate than the most static, less complex 3D organoid models. Since the approach can produce results within 12 days of the onset of the model, it allows for the rapid layout of patients with HAKs in correspondents and non -respondents and investigating non -standard NACT based on different chemotherapy factors for resistant patients in a clinically useful time. Findings are mentioned in Newspaper of translation medicine.
This patient -centered approach is based strongly on our previous successes using human organs chip technology to recap every individual TME of the patient from cancer outside their bodies, so that we can detect the combination of drugs that will work best for this very patient. This new way of approaching personalized medicine could be applied to clinical centers that focus on the care of patients suffering from many different types of cancer, such as the one run by our associates with patients with esophageal cancer. Perhaps equally important, it can also be used as a pre-clinical test to break the new soil in the development of treatments aimed at the tumor or layer for cancer patients and to allow the discovery of biomarkers that could be used to monitor and optimize their effects on them.
Donald Ingber, MD, Ph.D., Founding Director at the Institute of Biological inspirational Engineering Wyss at Harvard University
Ingber is also the Judah Folkman Professor of Vascular Biology at Harvard Medical School and Boston Children’s Hospital and the Hansjörg Wyss Professor Organically Inspired Engineering at the School of Engineering and Applied Sciences by Harvard John A. Paulson.
Modeling of esophageal pathologies
Ingber and Ferri teams have already cooperated in 2023 in a previous study in which they modeling Barrett’s esophagus on a petty bodily chip with vital support from the National Institutes of Health (NIH) and Cancer Research UK. The Barrett esophagus can be a malignant precursor to EAC, which is considered to be the result of a series of pathological changes that undergo the epithelial lining of the lower esophagus. These start with inflammation, which is most commonly caused by acid reflux, continue via The transformation of the esophageal tissue into a hyper-pranks stomach and a small intestine (Barrett’s esophagus) to eventually lead to the conversion of these extremely multiplier abnormal cells into cancer cells. It is important that these malignant changes are driven not only by molecular and cellular processes in the epithelial lining of the esophagus, but also to the underlying “layer”, which consists of fibroblast cells that communicate with cancer cells through a constant exchange of molecules and also contains blood flow.
“While in our previous work we faithfully recapitated the previous stages of the pathological process that might lead to the EAC, namely Barrett’s esophagus, our new study, we quickly promoted its cancer effect,” said second author Elee Shimshoni, Ph.D. “Only by reconstituting the basic ingredients of TME and imitation some of its fluid flows, which are normally provided by the fluid surrounding the cells (intermediate fluid) and the support of blood vessels, were able to obtain normally related to exposure to the drug and predict the NAc.
By patients in chips of cancer and rear
The team created the TME EAC chip, first creating personalized EAC organoids from biopsies taken endoscopically by a patient recently diagnosed with EAC but not yet treated. First writer Sanjima Pal, Ph.D. And other members of the Ferri team at the Health Center of McGill University, where Ferri is facing patients with esophageal cancer, had managed to create the ability to create esophageal organoids that match the patient with great consistency. The group then removed the organoids from the cultivation plate, broke them in their ingredients, cultivated cells in one of the two parallel channels of a microfibal chip of memory. and added fibroblasts associated with tumor from the same patients to the other channel to form a neighboring layer of tumor. Both channels are separated from a porous membrane, which allows cancer and strata tissues to exchange free molecules as they would in a real tumor. Finally, the researchers increased a cocktail of chemotherapy based on docetaxel in nutrients flowing through the strata channel, using drug concentrations and exposure times that reproduce a cycle of chemotherapy in patients with HAK.
For a group of eight patients, all EAC brands predicted their answers to NACT within 12 days. In four of the brands, chemotherapy caused EAC cells to die, while in the other four brands, EAC cells survived chemotherapy. These results were fully associated with patients’ responses to the same chemotherapy and their survival rates after EAC tumor resection.
Other writers in the study were Salvador Flores Torres, Mingyang Kong, Kulsum Tai, Veena Sangwan, Nicholas Bertos, Swneke Donovan Bailey and Julie Bérubé. It has funded a Grand Challenge regrograms (Cancer Research UK), which allowed a consortium of researchers, including Ingber and Ferri, focusing on the role of Stroma on the pathology of various diseases, as well as the General Hospital Foundation (LF).
Source:
Magazine report:
Pal, S., et al. (2025). The chip derived from the esophageal chip of the esophageal adenocarcinoma: a normal relevant platform for the functional oncology. Newspaper of translation medicine. Doi.org/10.1186/S12967-025-06593-1.