The fertility hormones FSH, LH, E2 and AMH are vital to reproductive health, influencing ovulation and egg development. Testing these hormones helps diagnose infertility and guide fertility treatments. FSH and LH stimulate follicle development and ovulation, while E2 (estradiol) is produced by follicle development. AMH assesses ovarian reserve. Testing is usually done during specific days of the menstrual cycle, with blood samples analyzed for hormone levels. This review addresses common questions about the importance and timing of fertility hormone screening.
We have covered these topics here
Which hormones are critical in assessing fertility?
When should fertility hormone testing be done?
What does an FSH fertility test reveal?
What are the ideal FSH/LH levels for conception?
How does estradiol affect fertility?
What does your AMH level mean in your fertility assessment?
What is the expected AMH level for different age groups?
When should women have hormone tests and how are they done?
In this webinar, an expert explained how to test hormones like FSH, LH, E2 and AMH for fertility. These hormones are important to women’s health and help doctors understand the ovaries and diagnose problems. They also help predict how women will respond to treatment.
FSH
FSH, a hormone that helps eggs develop, is checked with a blood sample on days 2-4 of a woman’s period.
- Normal levels are below 10 mU/ml.
- Higher levels may indicate age, menopause, or ovarian problems.
- Low FSH levels, along with low LH levels, can mean a problem in the brain.
FSH levels:
– Normal: Below 10 mU/ml
– Poor ovarian response: Between 10 and 20 mU/ml
– Low ovarian reserve: Above 20 mU/ml
Simply put, high FSH levels can happen as you get older, during menopause, or if your ovaries aren’t working well. Low FSH levels, along with low LH levels, can mean a problem in the brain. The brain produces hormones that tell the ovaries what to do. These hormones travel to the pituitary gland, where FSH and LH are produced. Both FSH and LH help create estrogen and progesterone in the ovaries. When estrogen and progesterone are low, FSH and LH can be high. This can happen during menopause when there is no estrogen in the blood.
Doctors use FSH to check how many eggs are left in the ovaries, but it’s not always the best test. It can change during the menstrual cycle and from cycle to cycle. So doctors usually do other tests to make sure they understand what’s going on. FSH also cannot tell if IVF will work.
Also read more about: Having trouble conceiving? Discover IVF with an egg donor!
LH
So, you know LH, right? It is short for luteinizing hormone. Well, guess what? It’s made in this part of the brain called the anterior pituitary gland. Fantastic, huh? Anyway, LH doesn’t work alone. It’s like a team player with another hormone called gonadotropin-releasing hormone, or GnRH for short. Together, they make things happen in your body.
Now, LH and this other hormone FSH, are like partners in crime. They help your ovaries grow these little things called follicles. But the real star of the show? Ovulation. LH has a leading role in making this happen. Do you know when you release an egg? This is thanks to LH.
Read more : How do ovulation test strips work? A comprehensive guide
But here’s the thing, catching LH in action isn’t always easy. Sometimes, it spikes – like, spikes really fast. But by the time you get a blood or urine test, it may have calmed down again. Hard, right? Usually, doctors check LH levels around days 2-4 of your period to catch it in action.
Now, in some cases, like if you have PCOS or if menopause is knocking on your door, LH can be on the higher side. But if your period has gone AWOL (that’s amenorrhea), LH might be playing it cool, hanging out on the low side.
Read more: Decoding 10 ovulation signs for parenthood
Estradiol
Let’s talk about estradiol—it’s a type of estrogen, one of those hormones that make us feel feminine, and more. So, where does it come from? Well, our ovaries have these little factories called follicles, and as they grow, they pump out estradiol.
Now, when we check your estradiol levels, we usually do it around days 2-4 of your period. Ideally, your levels should be between 25 and 70 pg/ml during this time. Estradiol works with FSH, another hormone, to give us a clearer picture of what’s going on inside your body.
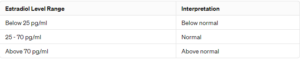
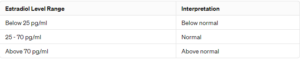
But here’s the thing – if your estradiol levels are high during this early part of your cycle, it can cause problems. It could mean that your ovaries will not respond well to treatment, making it harder to get pregnant. However, recent research suggests that it may not be as good at predicting problems as we once thought.
There is still some debate about whether estradiol can reliably indicate ovarian reserve—essentially, the number of eggs remaining. But it can still be useful to estimate if someone has a lower reserve than expected, especially if their FSH levels seem low because of high estradiol levels.
AMH
AMH, or Anti-Müllerian hormone, is a critical hormone for assessing ovarian reserve. It is a type of protein growth factor produced by special cells in the ovaries called granulosa cells, which are found in the small follicles called the antral and pre-manipulative follicles. These follicles are usually between 2 and 8 millimeters in size and may not always show up on an ultrasound.
AMH hormone range
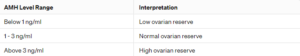
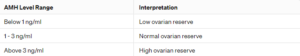
AMH plays a key role in regulating the recruitment of follicles, preventing them from being depleted all at once. Unlike some other hormones, AMH levels remain fairly constant throughout the menstrual cycle, meaning we can measure it at any time without worrying about fluctuations. However, what is considered a normal AMH level can vary depending on a woman’s age.
As women age and the number of follicles in their ovaries decreases, AMH levels also tend to drop. This decline is a normal part of aging. AMH levels also predict ovarian stimulation in procedures such as in vitro fertilization (IVF), giving us an idea of the number of eggs we are likely to retrieve. But remember, AMH isn’t about egg quality – it’s more about quantity. Age is still the best indicator of egg quality.
High AMH levels can increase the risk of ovarian hyperstimulation syndrome during IVF, so it is important to be careful with stimulation doses in these cases. On the other hand, low AMH levels are associated with a higher likelihood of treatment cancellation due to poor ovarian response. However, it is important to note that AMH levels are not a crystal ball for pregnancy outcomes or how quickly your ovarian reserve will decline.
Read more: Effect of age on pregnancy: Implantation and fertility
conclusion
In summary, hormone testing is extremely important to understand how well your ovaries are working to make babies.
LH and estradiol tests don’t tell us much about how many eggs you have left.
But checking your FSH levels between days 2 and 4 of your period is a big deal. When we combine this with the AMH test, we have a really good idea of how many eggs you might have. And these days, the AMH test is the best way to estimate your egg supply.
So if you’re thinking about starting a family or doing fertility treatment, getting your FSH and AMH levels checked can give you some really useful information about your chances of getting pregnant.
Read more about: Menstruation: Your Body’s Monthly Adventure Explained (Cycle Days)
FAQ
Q. Does high FSH always mean a woman is in menopause?
Not necessarily. You see, when a woman is in menopause, her FSH level can be around 50 or even higher. So, if someone’s FSH level is that high, it can indicate menopause. But if it’s around 25, it doesn’t automatically mean menopause. It suggests that her ovaries may not have many eggs. The timing of the FSH test is of great importance. For example, testing towards the end of her menstrual cycle could mean something different. So while a very high FSH level of 50 or more could mean menopause, not all FSH levels do.
Q. Can I increase my egg supply naturally?
No you can not. When women are born, they have many eggs in their ovaries. As they grow, the number of eggs decreases. Right now, there is no way to increase the number of eggs you have. Living healthy can help your ovaries stay healthy, but it won’t produce more eggs. Scientists are studying ways to help women with low egg supply, but these methods are not yet ready.
Q. How can I improve my hormones to have a baby?
You don’t need to do anything special to improve your hormones. The most important thing is to have a regular egg supply and make sure your ovaries are working well. When you have fertility treatment, your doctors give you medicine to help your ovaries make more eggs. This medicine helps the eggs grow better, giving you a better chance of having a baby.
Q. Can taking certain vitamins make my eggs healthier?
Some vitamins might help, but we’re not sure. We are not sure if certain vitamins can improve egg quality, although they are believed to protect the ovaries. Taking these vitamins is safe, but they may not make much of a difference in the quality of your eggs.
Q. Can hormone tests show if my eggs are good?
Not really. Hormone tests can tell us about your egg supply, but they don’t tell if your eggs are good. Your age is the most important thing about egg quality. Older women usually have lower quality eggs. To check if your eggs are good, doctors look at how the embryos develop in the lab after they are fertilized.
Q. Does stress make my eggs worse?
Not immediately. Stress can affect your hormones and your period, but it usually doesn’t reduce your egg supply. Prolonged stress can negatively affect your overall health, indirectly affecting your eggs.
Q. What do LH and FSH levels tell us about fertility?
LH and FSH levels can tell us if your hormones are balanced. Sometimes, if you have too much LH compared to FSH, it can mean a problem like PCOS. But it’s not the only thing we look at to understand your fertility.
