• Research Highlights
A persistent state of anger or annoyance combined with frequent and intense outbursts of anger in children and adolescents often signals clinically reduced irritability. Clinical irritability disrupts the child’s daily life and may continue to cause problems in adulthood. Although irritability is one of the main reasons children seek psychiatric care, it has not been studied in comparison to other childhood disorders. Essentially, evidence-based treatments for clinical irritability are also lacking.
In a new study, researchers at the National Institute of Mental Health (NIMH) successfully used exposure-based cognitive behavioral therapy (CBT) to treat severe irritability in children. This promising finding highlights the importance of individualized interventions in this area of child psychiatry.
What is severe irritability in children?
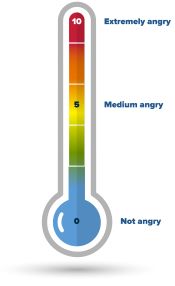
This study focused on severe and disabling outbursts of irritability and temper in youth. All children feel angry or irritable at times. Severe irritability is more serious and can cause problems at home, during school and with friends.
Irritability and outbursts are part of many mental disorders, but they are key symptoms disruptive mood disorder (DMDD). DMDD is diagnosed in children and adolescents who exhibit constant irritability, frequent anger, and intense outbursts of anger.
The symptoms of DMDD are serious and require treatment. Children with this high level of irritability often get angry and to a degree disproportionate to their situation and age. When angry, they have temper tantrums, which usually involve high motor activity and verbal or physical aggression. These children are also persistently irritable or cranky most of the time and in many situations.
How did researchers deal with severe irritability in children?
Researchers led by Melissa Brotman, Ph.D., in the NIMH Brain Research Program tested a new treatment for irritability. It was developed in the laboratory of Dr. Brotman, the exposure-based CBT therapy is based on a highly effective treatment for anxiety—exposure therapy. In this pilot study, researchers examined the effectiveness, acceptability, and feasibility of exposure therapy for severe irritability.
Forty children (8–17 years old) participated in the study, which took place in NIH Clinical Center . Children had to have at least one of the two core symptoms of DMDD: chronic irritability or intense anger outbursts. Some children also had co-occurring anxiety or attention-deficit/hyperactivity disorder (ADHD), but were ineligible for participation if diagnosed with other disorders, such as bipolar disorder, substance use disorder, schizophrenia, or autism spectrum disorder.
All children received 12 sessions of exposure-based CBT according to an established manual written by Drs. Brotman. Each treatment session had one child and one parent.
- The children’s section focused on increasing frustration tolerance. Clinicians carefully exposed children to situations that elicited anger, gradually progressing through a hierarchy specific to that child. Examples could be removing a preferred object (for example, pausing a video game or getting off the iPad) or starting an unpleasant activity (for example, brushing teeth or doing homework). Clinicians worked with the child to learn to tolerate and respond constructively to their emotions without throwing tantrums.
- The parenting section focused on parent management skills. Parents were taught to actively ignore their child’s tantrums to stop reinforcing these behaviors. Instead, they learned how to focus on and consistently reward positive behaviors.
Children were randomized to follow-up for either 2, 4, or 6 weeks before starting treatment. Clinical observers were blinded to when active treatment was initiated. This observation period allowed the researchers to confirm that symptoms changed only after treatment began and were not accounted for by clinician expectations of treatment.
Clinicians, children, and their parents rated the child’s irritability symptoms and overall functioning during the observation period, during treatment, and 3 and 6 months after treatment. Depression, anxiety and ADHD symptoms were also assessed for comparison. Acceptability, feasibility, and safety of the treatment were determined by study dropout and adverse event rates.
Did exposure-based CBT help children with severe irritability?
Irritability symptoms were significantly reduced during treatment based on clinician, child, and parent reports. Overall functioning also improved—at the end of treatment, 65% of children were significantly improved or recovered based on clinician measures. Symptoms did not return after treatment was discontinued and, in fact, treatment gains were maintained at 3- and 6-month follow-up.
When examining core DMDD symptoms, 60% of children were considered recovered on the Temperament scale and 25% recovered on the Irritable Mood scale at the end of treatment. This result suggests a stronger effect of exposure therapy in reducing angry outbursts compared to improving irritable mood. In contrast, the treatment was not associated with significant changes in anxiety, depression, or ADHD symptoms, suggesting its specificity in targeting irritability.
No families dropped out of school once treatment began, suggesting that exposure therapy was acceptable and feasible. Likewise, no adverse effects were reported, supporting the safety of using exposure therapy with children.
What can researchers do after further treatment for children with severe irritability?
Taken together, these results support the efficacy, acceptability, and feasibility of exposure therapy for youth with severe irritability. Irritability symptoms and overall functioning improved during treatment per clinician, child, and parent report and were maintained for several months after treatment was discontinued.
This study has some limitations. First, it had a relatively small sample size with limited racial, ethnic, and socioeconomic composition, which limits the generalizability of the results. Second, the study did not include a control group of untreated children with irritability. Although the researchers addressed this concern by having multiple observation periods, comparing this new treatment with current clinical care is a critical next step. Third, the study included a wide age range, making it important to test whether there are differences in outcomes based on age. Finally, because clinicians delivered the child and parent components simultaneously, future studies could examine the individual contribution of child exposure therapy to parent management skills to determine whether one drives treatment outcomes.
The positive results from this pilot study set the stage for further investigation of CBT treatment for childhood irritability. Although the treatment is not yet ready for clinical practice, it offers one of the few evidence-based treatments for this common and disabling childhood disorder. Researchers plan to test and refine exposure therapy in larger, more controlled clinical trials to advance treatment for severely irritable children and their families.
Report
Naim, R., Dombek, K., German, RE, Haller, SP, Kircanski, K., & Brotman, MA (2023). An exposure-based cognitive-behavioral therapy for youth with severe irritability: Feasibility and preliminary efficacy. Journal of Clinical Child & Adolescent Psychology. https://doi.org/10.1080/15374416.2023.2264385
