The increasing incidence of cancer worldwide has led to an increasing number of surgeries involving lymph node removal. Although these procedures play an important role in staging cancer and preventing the spread of malignancies, they sometimes have serious long-term consequences. Since lymph nodes do not naturally regenerate after they are removed, their absence can lead to a condition known as secondary lymphedema. It manifests as chronic swelling, discomfort and reduced mobility in affected limbs or areas, seriously affecting the patient’s quality of life.
Consequently, an important focus in the field of regenerative medicine is the development of strategies to repair or regenerate damaged lymphatic structures to effectively treat secondary lymphedema. Existing approaches have largely focused on stem cell and lymphoid tissue transplantation. However, these techniques often require complex conditioning protocols and, more importantly, have shown limited efficacy in improving the core clinical symptoms of lymphedema.
In this context, a research team led by Associate Professor Kosuke Kusamori from the School of Pharmaceutical Sciences at Tokyo University of Science (TUS), Japan, is pioneering an innovative technique for lymphatic tissue engineering that could revolutionize the treatment of secondary lymphedema. Their study, published in volume 16 of the journal Nature communications on November 19, 2025, describes a simple protocol for producing engineered lymph tissue that can restore lymph flow after lymph node removal. This work was authored by second year PhD student Mr. Shu Obana, Assistant Professor Shoko Itakura and Professor Makiya Nishikawa, also from TUS.
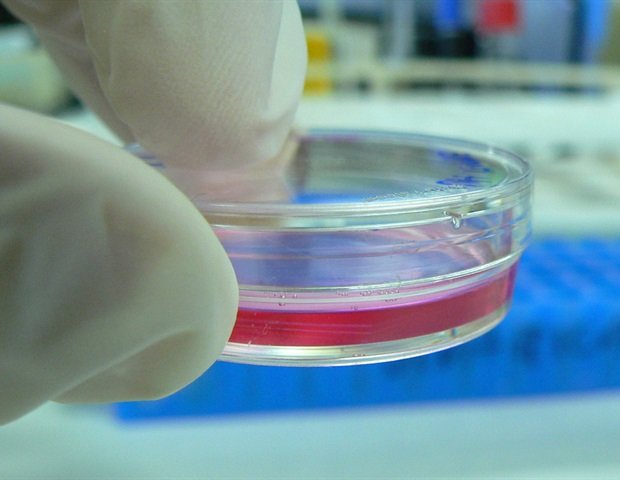
The proposed approach is based on a novel centrifuged cell stacking technique for tissue replacement bioengineering for surgically removed lymph nodes. First, the researchers placed mesenchymal stem cells (MSCs), which are known to support tissue regeneration and provide structural scaffolds, into the wells of a Transwell culture plate. By centrifugation of the whole plate, the MSCs settled uniformly to the bottom of the wells, forming a first layer. The researchers then added lymphatic endothelial cells to the wells, followed by another round of centrifugation to spread them evenly as a second layer. Finally, after a final centrifugation step after MSCs were added again, the result was a three-layer cell structure, which the researchers called centrifuge-based engineered lymph tissue (CeLyT).
Using an animal model of lymphedema, the team regenerated a functional lymph node that showed structural similarity to the native lymph node. They confirmed that transplanting CeLyTs restored lymph flow in mice whose popliteal and inguinal lymph nodes on the right lower limb had been removed. As a result, these mice showed a marked improvement in lymphedema symptoms, with the thickness of their legs and feet returning to normal within weeks. In addition, mice treated with CeLyTs also showed recovery of infiltration capacity and immune cell populations such as T cells and macrophages, and lower adipose tissue accumulation in the affected areas, reaching levels similar to normal mice.
The researchers carefully analyzed the structures formed after CeLyT transplantation to shed light on the observed therapeutic effects. “CeLyTs may initially induce the formation of lymph and blood vessels around the transplant site, leading to the creation of an immature lymph node-like structure formed by the incorporation of host-derived cells into the tissue within several days, followed by its maturation and ability to function as a lymph node within 10 days after transplantation,” explains Dr. Kusamori.
This study marks the world’s first successful regeneration of fully functional lymph nodes via cell transplantation, offering a promising treatment option for patients who develop lymphedema following oncological operations involving lymph node dissection. Economically, a single transplant could provide long-term therapeutic benefits, significantly reducing the cumulative costs associated with repeated hospital visits and long-term use of compression garments. Taken together, these results highlight the powerful therapeutic potential of introducing appropriately engineered tissue into the lymphatic system, surpassing the efficacy of current treatment options for lymphedema.
“Although compression therapy represents the gold standard for the treatment of lymphedema in clinical practice, it usually delays swelling in the legs of mice with lymphedema. In contrast, CeLyTs were more effective in suppressing lymphedema, also showing strong therapeutic effects even in a more severe model of chronic lymphedema,” observes Dr. Kusamori.
In addition, CeLyTs demonstrated greater lymphedema suppressive activity, compared to engineered tissues constructed by other tissue engineering methods.“
Kosuke Kusamori, Associate Professor, School of Pharmaceutical Sciences, Tokyo University of Science
Hopefully CeLyTs will translate into clinical practice!
Source:
Journal Reference:
Obana, S., et al. (2025) Reconstruction of the lymphatic system by transplantation of a centrifuge-based engineered lymphoid tissue. Nature communications. DOI: 10.1038/s41467-025-65121-3. https://www.nature.com/articles/s41467-025-65121-3.