Doctors examined stool transplants from bowel bacteria in hospital patients. Could this be the next tool to combat fatal drug resistant infections?
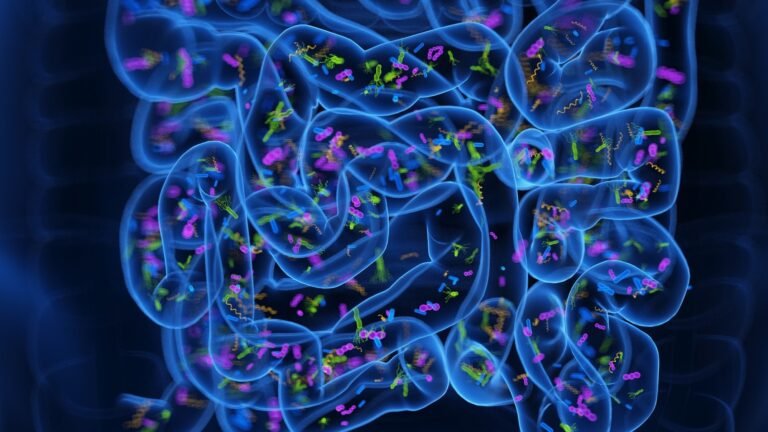
Study: Germ transplantation between patients receiving long -term care. Credit Picture: 3DMEDISPERE/Shutterstock.com
A non -randomized clinical trial that examines the safety and acceptance of the transplantation of germ fecal in patients with long -term hospital care has revealed that the intervention is safe and well tolerated. A detailed test report is published in Open the Jama Network. This could potentially reduce some effects associated with infection, although in this pilot study, all recipients remained colonized with at least one multiple -medication resistant body during follow -up.
Background
Multiple -resistant microbial colonization in the intestine is associated with an increased risk of systemic infection and transmission, especially in patients receiving long -term care in hospitals while recovering from critical diseases. However, the US Food and Drug Administration (FDA) has not approved effective interventions to manage these terms.
Emerging indications show that microbial interventions, such as the transplantation of microbial fecal, are explored for their ability to reduce the risk of infection, the duration of antibiotic treatment and hospital stay in patients with intestinal microbiocide resistant microbioches. However, the results have been mixed in different patient arrangements and populations and some previous elements come from indirect findings or groups not exclusively colonized with MDROS.
In this non -central clinical trial, the researchers investigated the safety and acceptance of germ transplantation in patients with long -term hospital care.
Test planning
The test was involved in 42 patients with intestinal microbial colonization from a long -term acute care hospital in Atlanta, Georgia.
Of the registered patients, 10 received microbiotic fecal feces from healthy donors through gastrostomy or enema without air conditioning antibiotics or bowel preparations. The remaining 32 patients were the control group and did not receive germ transplantation.
The frequency and severity of the side effects associated with the transplantation of germs were evaluated and compared to those of the control group. The ratio of patients with positive effects of MDRO cultivation after six months of transplantation was also evaluated.
Trial findings
Evaluation of safety during six -month monitoring revealed that the germ transplantation is not related to any serious side effects. The side effects reported after the transplant were generally mild.
The most remarkable non -severe adversity in a patient was vomiting after the administration of the germ of the stool through the gastrostomy tube. Two patients died after transplantation. However, deaths were not related to transplantation, but instead were associated with the medical complexity of patients.
Evaluation of intestinal microbial colonization has revealed that patients with germ transplantation have fewer episodes of systemic bacterial infection, reduced pathogen intestinal domination and fewer days of antibiotic treatment than patients. Still, these findings were exploratory, based on post -HOC analyzes, and not statistically significant.
Compared to 19% of control patients, none of the recipients of germ transplantation had positive blood crops six months after treatment, although this difference did not reach statistical significance.
Despite these tendencies, all germ transplant recipients remained positive for at least one MDRO in monitoring comprehensive crops and 60% acquired a new MDRO category during the study.
Meaning
The test findings indicate that healthy germal germs derived from a donor given through gastrostomy or instillation of the seconds are well tolerated and safe for patients with long -term hospital care with intestinal microbial colonization resistant to multiple drugs.
The test also suggests that transplantation of stool germ may reduce systemic bacterial infection, intestinal pathogen domination and the use of antibiotics in this high -risk population. However, the small sample size and the design of the study of definitive conclusions about efficiency.
Intestinal colonization MDRO increases the risk of systematic and urinary tract. Existing elements emphasize the importance of transplanting germs in reducing mortality, systemic infection and utilization of healthcare, even among patients with persistent cultivation effects that are positive for microorganism. This study also observed an increased microbial diversity of the bowel among the recipients of microbial fecal transplantation, indicating a possible displacement of germs despite persistent colonization.
The current test highlights the acceptance, safety and possible efficacy of a single germ transplant. These pilots emphasize the need for further large -scale clinical trials to explore whether increased doses, more frequent doses or antibiotic or laxatives preparation can more effectively prevent microbial colonization in the intestine.
Given the current non -availability of FDA’s approved treatments, the optimization of germ preparation and dosage strategies would be particularly beneficial for long -term acute care hospitals and other healthcare facilities facing high -prevailing patients.
Patients were not accidentally assigned to the intervention and control groups in this test and the treatment was not hidden. Future tests should consider these factors for a more decisive interpretation.
The test measured the results associated with treatment using quality cultivation methods, with positive or negative results. Therefore, it could not provide information on possible quantitative reductions in pathogens after transplantation of germs.
Long -term care hospitals are at greater risk of mortality from various medical complications and require frequent empirical antibiotic therapies. In addition, the weight of colonized patients, especially with multiple bacterial resistant, in a hospital unit further increases the risk of acquiring new microbial colonization after transplantation of microbial fecal. These competitive risks may cause clinical outcomes related to intervention.
The evolution of colonization in infection is relatively rare in many populations, making this a difficult end. The study of interventions in patients with higher prevalence and colonization in the development of infection increases the effectiveness of measuring these critical final points, but may increase the incidence of competitive risks with many results of safety and efficiency.
As the researchers said, these restrictions are offset by the demonstration of the sorting of the sorting of microbial interventions with prevalence sampling throughout the installation followed by targeted treatment.