White blood cells or leukocytes are the body’s first and second lines of defense against foreign organisms and particles. However, few drugs target the production and movement of these cells for clinically useful purposes. A new study published in the journal Immunity, immunity explores the signaling molecule landscape to identify potential targets for leukocyte migration into the bloodstream.
Study: Inhibition of the small molecule histone acetyltransferase CBP/p300 mobilizes leukocytes from the bone marrow through the endocrine stress response. Image credit: Rost9 / Shutterstock
Leukocytes, including neutrophils, monocytes, and B lymphocytes, are formed in the bone marrow from blood-forming precursor cells and in some other specialized organs. They are stored in the bone marrow until they are released into the circulation.
There are two compartments of leukocytes in the blood and peripheral tissues, which exhibit changes in size with varying physical conditions. For example, when the body is injured, stressed, or infected, the number of white blood cells in the affected tissue changes and returns to normal once the threat is contained.
Multiple regulatory steps are involved in the breakdown of leukocytes as well as their movement to different sites where they are needed. These originate in the central nervous system (CNS) in response to peripheral signals, and are regulated by neural circuits involving both the sympathetic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis.
These signals work to increase bone marrow hematopoiesis, recruit leukocytes into the blood and other tissues where they are needed, and ensure that they return to normal levels once the challenge is over.
In some diseases, this homeostatic control is lost, thus leading to abnormal numbers, such as bone marrow failure on the one hand or acute leukemia on the other. So far, however, few drugs can help correct this dysregulation by modifying the rate of leukocyte production, breakdown, or migration, whether in blood cancer, chronic inflammation, or acute hyperinflammatory conditions.
Among the drugs available are the granulocyte colony-stimulating factor (G-CSF) family, CXC-motif chemokine receptor 4 (CXCR4) antagonists, such as plerixafor/AMD3100), or integrin very late antigen 4 (VLA4) inhibitors ). G-CSF is used, for example, to correct neutropenia in patients undergoing chemotherapy, but is less useful in patients with acute febrile conditions involving low neutrophil counts. In addition, G-CSF can cause side effects in some patients.
The need to learn more about this field of pharmacology led the present study. It focuses on a small molecule called E1A-related protein p300 (EP300 or p300), which appears to be newly acquired during the leukemic phase of a condition called severe congenital neutropenia (SCN).
Loss of function of this gene resulted in reduced production of blood cells if deleted before birth, but high or leukemic leukocytes in later life. This has a homologous cyclic-adenosine-monophosphate-response-element-binding protein (CREBBP, also known as “CBP”, with 90% sequence homology. One of the 8 domains in this gene is responsible for histone acetyltransferase (HAT ) activity and contains a mutation in the SCN that causes leukemic transformation.
In this case, this domain may be able to produce “leukocytosis on demandchanging the sizes of different leukocyte compartments.
What did the study show?
The scientists found that inhibition of the CBP/p300 domain with its HAT activity by the small molecule inhibitor A485 resulted in reversible competitive inhibition of HAT enzyme activity, specifically for CBP and p300 compared to other HATs. As expected, this led to a rapid increase in acetyl CoA levels in bone marrow macrophages in mouse models. The result was rapid leukocytosis.
This was found to be a dose-dependent effect and did not diminish with repeated administration. When another type of CBP/p300 HAT inhibitor (C646) was used, the same effect was observed, confirming the mechanism of action. In contrast, inhibitors of DNA binding by the protein or other HAT found in mammals failed to induce leukocytosis.
Blood levels of A485 rose rapidly when it was injected into the mice, accumulating in the bone marrow, adipose tissue, liver, spleen and kidney, but not in the brain. The number of leukocytes increased in parallel, including neutrophils, lymphocytes and monocytes. One week later, no evidence of drug administration was observed, suggesting a transient effect.
The increase in leukocyte count was comparable to that achieved by G-CSF, although somewhat faster for neutrophils. When both were given, significantly higher neutrophil counts resulted. However, after 24 hours, all three blood cell types were increased with G-CSF versus A485.
This indicates a smaller and different effect of A485 compared to G-CSF.
To extend the observations to humans, the researchers looked at data from a group of patients with a rare disease called Rubinstein-Taybi syndrome (RSTS), where CREBBP and EP300 mutations occur. About two-thirds had high leukocyte counts, with 70% showing mutations in the HAT domain. As expected, this group was more likely to develop leukocytosis than the other group, where HAT was spared.
Does this observation have clinical utility? To find out, they tested the effect of A485 on a group of mice with myelodysplastic syndrome (MDS), finding that the small molecule kept white blood cell counts normal. Second, they induced severe neutropenia with a course of chemotherapy in a mouse model, showing that A485 led to an acute recovery of leukocyte counts.
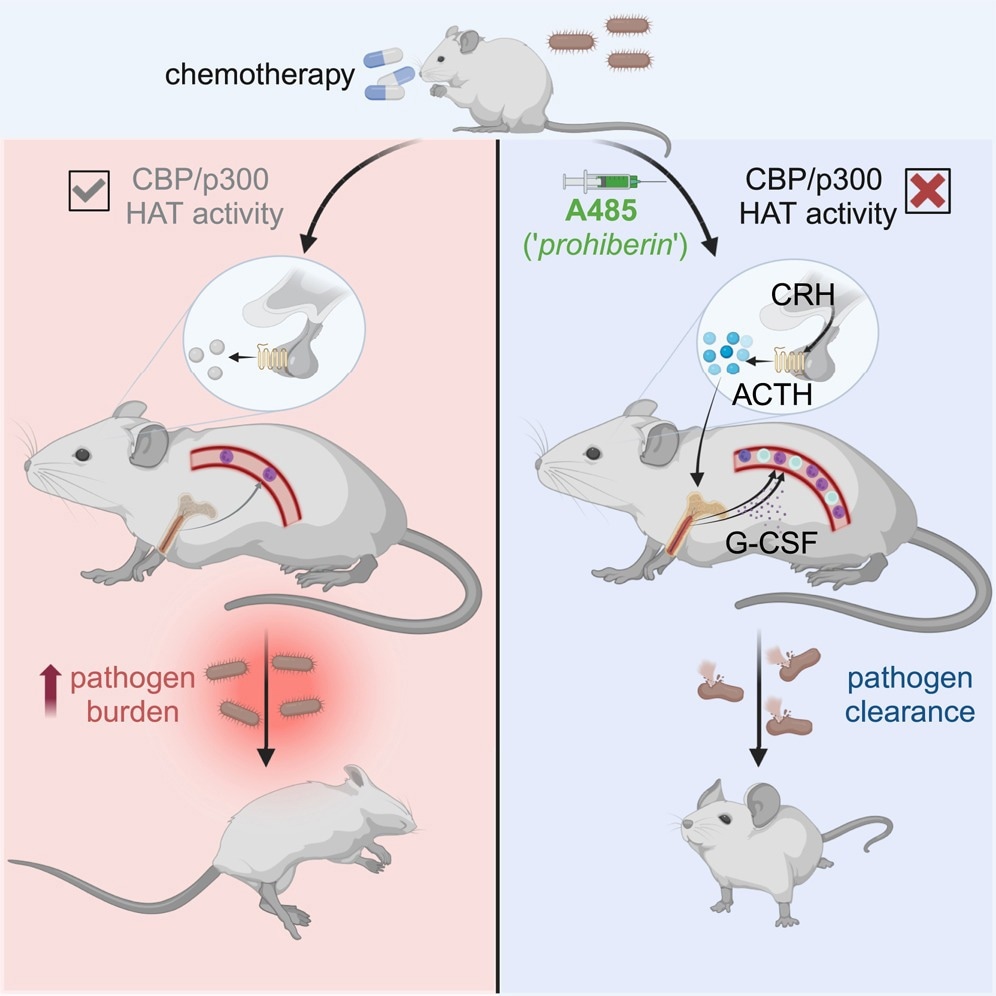
Then they introduced the organization Listeria monocytogenes at a dose that induces sepsis in chemotherapy-induced pancytopenia mice. Neutrophils are vital for the immune defense against this microbe. After initiation of infection, they injected A485 versus vehicle in controls.
While those treated with vehicle became sick and died from sepsis, A485 in a single dose led to improved survival, with fewer bacteria recovered from treated animals. A485 mobilizes leukocytes from the bone marrow, which is the mechanism of leukocytosis. In contrast, there was no emergent hematopoiesis in the bone marrow.
Different leukocyte subsets responded to distinct pathways activated by A485. These include both G-CSF-dependent and -independent pathways of neutrophilia, but other pathways for lymphocytosis.
In addition, A485 uses neurohumic pathways, specifically the HPA axis, to induce leukocytosis, as shown by increased blood glucocorticoid levels after A485 administration. However, the leukocytosis response induced by HPA activation is not glucocorticoid-dependent, but occurs in response to CRHR1-regulated signals, including adrenocorticotropic hormone (ACTH), occurring with the loss of HPA feedback signals.
While neutrophils increase with ACTH administration, lymphocyte numbers increase only with glucocorticoid blockade, indicating that the two are regulated differently.
What are the consequences;
“Competitive, reversible, small-molecule-mediated inhibition of the CBP/p300 HAT domain triggers acute and transient leukocyte mobilization from the bone marrowFurther research is needed to determine which clinical settings are ideal for this drug. A485 may be better if only a quick short increase in neutrophils is required, whereas long-term recovery of blood cell production in the bone marrow may require G-CSF.
The timing of administration must also be determined for good results, as patients with neutropenic sepsis present at various time points and stages. Furthermore, the value of such drugs in bacterial or viral, rather than listeric, sepsis remains unexplored.
However, as reported by previous researchers, it has anticancer effects, which could make it valuable in adjuvant therapy for cancer patients. The current study also sheds light on the role of ACTH, rather than its downstream products, glucocorticoids, in leukocyte homeostasis and G-CSF activity.
