In a recent study published in Nature Microbiologya group of researchers investigated its clinical significance Streptococcus agalactiae (Group B Streptococcus, GBS) deoxyribonucleic acid (DNA) in the placenta in relation to neonatal unit (NNU) admission and morbidity in term infants.
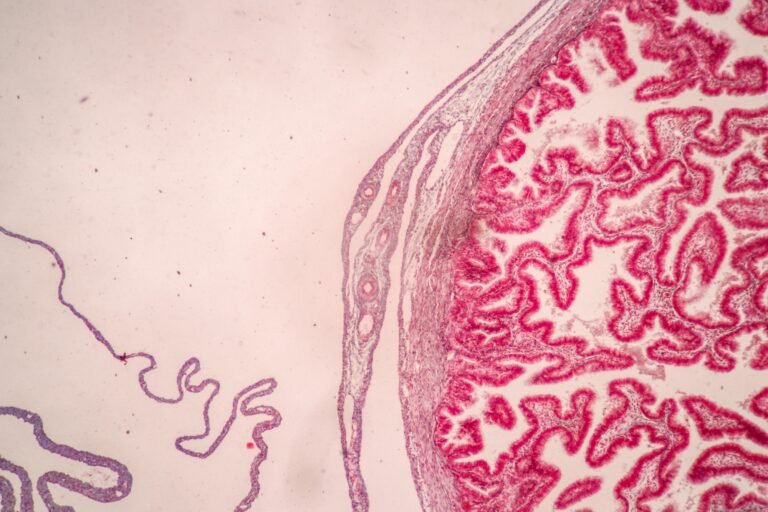
Study: Streptococcus agalactiae placental DNA is associated with neonatal unit insertion and fetal proinflammatory cytokines in term infants. Image credit: Rattiya Thongdumhyu/Shutterstock.com
Record
GBS is the common cause of neonatal sepsis in the first week of life, known as early onset disease (EOD). About 20% of women carry GBS in their genital tract, and without intervention, about 1% of infants from these women develop EOD.
In 2020, approximately 20 million pregnant women were GBS carriers, resulting in 230,000 cases of EOD and contributing to approximately 50,000 stillbirths and 50,000–100,000 infant deaths worldwide. In high-income countries, EOD is a rare phenomenon, while it occurs quite frequently in low-income countries, although data are less precise.
Previous metagenomics research identified GBS as the only bacterium in the antepartum placenta in full-term pregnancies. Further research is needed to fully understand the mechanisms by which the presence of GBS in the placenta leads to neonatal morbidity and to develop targeted interventions for prevention and treatment in diverse global settings.
About the study
The present study used data and samples from a prospective cohort of unselected nulliparous singleton females receiving antenatal care at the Rosie Hospital in Cambridge, United Kingdom (UK), from 2008 to 2013.
The only exclusion criterion was multiple pregnancies. Women were recruited around the time of their appointment ultrasound, usually around 12 weeks’ gestation, and followed up with study visits at 20, 28, and 36 weeks’ gestation.
After delivery, technicians routinely took samples from the placenta, umbilical cord and fetal membranes. These samples were immediately frozen for molecular analysis and fixed for microscopy. In addition, umbilical cord blood was collected from about a third of the participants.
Outcome data for the study were comprehensively collected, including individual review of maternal medical records and linkage to various electronic databases containing clinical information, with results from all microbial cultures performed during pregnancy.
A pregnancy outcome prediction (POP) study was conducted with a sample size of 4,212 women. Height, median age, body mass index (BMI) and interquartile range were recorded.
Ethical criteria were followed for the research, which was approved by the Cambridgeshire Research Ethics Committee 2 under reference number 07/H0308/163. Written informed consent was obtained from all participants and ethical requirements were adhered to.
Study results
In this reanalysis, the focus was on 436 fetuses defined as NNU admission cases within 48 hours and beyond 48 hours after delivery. Results showed that 23.3% of full-term infants with placental GBS DNA and 8.4% without were admitted to NNU.
This showed a significant association between placental GBS DNA and NNU admission, even after adjustment for maternal characteristics.
This was followed by another validation study involving non-overlapping 239 NNU admission cases and 686 condition control groups drawn from the same cohort. The present study replicates the results of the first, revealing the association of GBS placental DNA with the increasing prevalence of NNU imports.
Further analysis distinguished septic from non-septic phenotypes of neonatal morbidity. This study categorized NNH admissions according to clinical evidence of sepsis, from none to confirmed GBS sepsis.
Placental GBS was significantly associated with NNU admissions, where probable, culture-negative and proven GBS sepsis were considered as outcome measures. Pathological findings in fetal membranes and umbilical cord were strongly associated with placental GBS DNA in cases accompanied by chorioamnionitis and mycosis.
The other aspect the study looked at is the rates of placental GBS associated with colonization of the genital tract. It found a higher prevalence of GBS-positive placentas in participants with a positive high vaginal smear (HVS) for GBS during pregnancy compared to those with a negative HVS or no HVS culture.
The researchers also showed no relationship between the detection of GBS DNA in the placenta and the timing of deliveries or delivery methods. Furthermore, additional tests to validate the GBS DNA marker, which included a novel reverse transcriptase-quantitative polymerase chain reaction (RT-qPCR) assay for GBS 16S ribosomal ribonucleic acid (rRNA), demonstrated that such findings were reliable.
Analysis of proinflammatory cytokines in cord serum from deliveries with GBS-positive placentas revealed a “cytokine storm”—a significant increase in cytokines—compared to GBS-negative cases. This suggests an exaggerated inflammatory response to the pathogen.
Finally, the study detailed the clinical features of cases with proven and probable GBS sepsis. It found that only a minority of these cases were detected with prenatal GBS colonization or received antibiotics at delivery.
This highlighted the potential under-recognition of GBS-related neonatal morbidity and the need for better screening and preventive measures. The presence of GBS DNA in the placenta is strongly associated with an increased risk of neonatal morbidity, evidenced by NNU insertion.
This association was not only consistent across different analytical methods, but also highlighted the possibility of an exaggerated inflammatory response in neonates, leading to severe outcomes.
The study findings have important implications for clinical practice, particularly regarding the screening and treatment of GBS in pregnant women.