A single exposure to a toxic fungicide during pregnancy can increase the risk of disease for 20 subsequent generations – with inherited health problems worsening many generations after exposure.
Those are the findings of a new University of Washington study in rats that expands understanding of how long the transgenerational effects of toxic exposure can last, as they are transmitted through changes in reproductive cells. The study, published this week in Proceedings of the National Academy of Scienceswas written by WSU biologist Michael Skinner, who has been studying this “epigenetic transgenerational inheritance” of disease for two decades.
The research has implications for deciphering the increasing rates of disease among humans, Skinner said, suggesting that the reason someone has cancer today may be due to an ancestor’s exposure to toxins decades earlier. On the other hand, epigenetic research has also revealed potential treatments by identifying measurable biomarkers for disease that could ultimately drive preventive treatments.
This study actually says that this is not going to go away. We have to do something about it. We can use epigenetics to move us away from reactive medicine and toward preventive medicine.”
Michael Skinner, professor in the School of Biological Sciences and founding director of the Center for Reproductive Biology
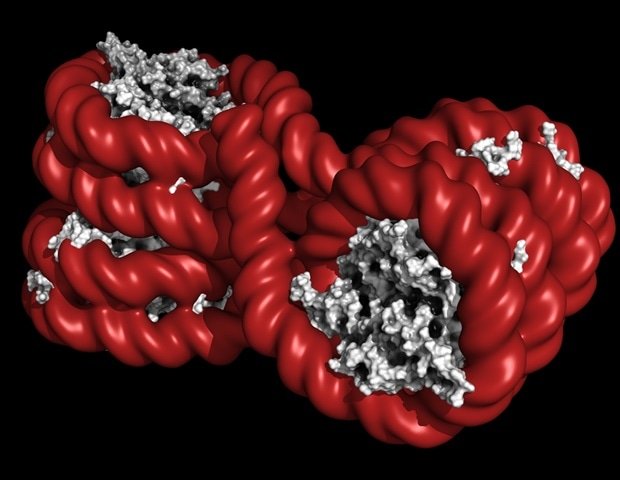
Skinner first identified epigenetic inheritance of the disease in 2005 and has since published dozens of papers. The effects are transmitted through changes in sperm and eggs – the germline – and previous studies have shown that the incidence of inherited disease may be higher than that resulting from direct exposure to toxins.
“Essentially, when a gestating female is exposed, the fetus is exposed,” he said. “And then the germline within the embryo is also exposed. From that exposure, the offspring will have potential effects of the exposure, and the great offspring, and so on. Once it’s programmed into the germline, it’s as stable as a genetic mutation.”
Recently, Skinner’s lab sought to determine how long these effects last and whether disease risk changes over generations.
In a study published late last year, Skinner’s team examined 10 generations of rats after an initial exposure to vinclozolin, a fungicide used primarily in fruit crops to control mold, mildew and rot. The increased prevalence of the disease persisted in these generations.
The current paper, published in Proceedings of the National Academy of Sciencesdoubled the number of generations studied, showing similar persistence of the disease in the kidneys, prostate, testes and ovaries, as well as other health effects. Furthermore, from later generations, mothers and offspring began to die in large numbers during the birth process.
“The presence of the disease remained almost the same, but around 15u generation, what we started to see was an increased disease state,” Skinner said. “By the 16th, 17th, 18th generation, the disease became very apparent and we started seeing abnormalities in the birth process. Either the mother would die, or all the puppies would die, so it was a really lethal kind of pathology.”
Skinner said he reduced the dose of the toxin conservatively, to a level below what the average person can consume in their diet.
The paper was authored by Eric Nilsson, Research Professor in the School of Biological Sciences. Alexandra A. Korolenko, a former graduate student and now a postdoctoral researcher at Texas Tech University, who was the lead author. and Sarah De Santos, an undergraduate research assistant in the Skinner lab.
Skinner said epigenetic disease inheritance could explain rising rates of chronic disease in humans, an increase that paralleled the increasing use of pesticides, fungicides and other environmental chemicals in agriculture and other industries. More than three-quarters of Americans now deal with a chronic disease, such as heart disease, cancer or arthritis, and more than half have two diseases, according to the US Centers for Disease Control.
Research by Skinner and others has found epigenetic alterations in human germ lines that correspond to studies in mammals and the increased incidence of disease in humans with transgenerational effects found in animal studies.
The scale of the time period involved is daunting. Twenty generations in rat populations cover a few years. in humans, it’s more like 500. With such a long time between potential cause and effect, how could the effects of exposures be mitigated?
Skinner pointed to another product of epigenetic research as a possible answer: the discovery of epigenetic biomarkers that predict susceptibility to specific diseases. Developing the use of epigenetic biomarkers to promote preventive therapies in humans could provide a valuable strategy to offset long-term effects.
“In humans, we actually have epigenetic biomarkers for about 10 different disease susceptibilities,” he said. “It’s not saying you have the disease now, it’s saying 20 years from now, you will potentially have the disease. There are a whole host of preventive medical approaches that can be taken before the disease develops to delay or prevent the onset of the disease.”
Source:
Journal Reference: