For more than a century, Alzheimer’s disease (AD) has been considered irreversible. Consequently, research has focused on preventing or slowing the disease rather than curing it. Despite billions of dollars spent on decades of research, there has never been a clinical trial of an AD drug aimed at reversing the disease and restoring function.
Now, a research team from University Hospitals, Case Western Reserve University and the Louis Stokes Cleveland VA Medical Center has challenged this long-held dogma in the field. They tested whether brains already severely affected by advanced AD could recover.
The study, led by Kalyani Chaubey, PhD, from the Pieper lab, published today in Cell Reports Medicine. By studying various preclinical mouse models and human AD brains, the team showed that the brain’s failure to maintain normal levels of a central cellular energy molecule, NAD+is an important driver of AD, and that maintaining proper NAD+ Balance can prevent and even reverse disease.
NAD+ Levels naturally decline throughout the body, including the brain, as people age. No proper NAD+ balance, cells eventually become unable to perform critical processes required for proper function and survival. In this study, the team showed that the reduction of NAD+ is even more severe in the brains of people with AD, and that this is also the case in mouse models of the disease.
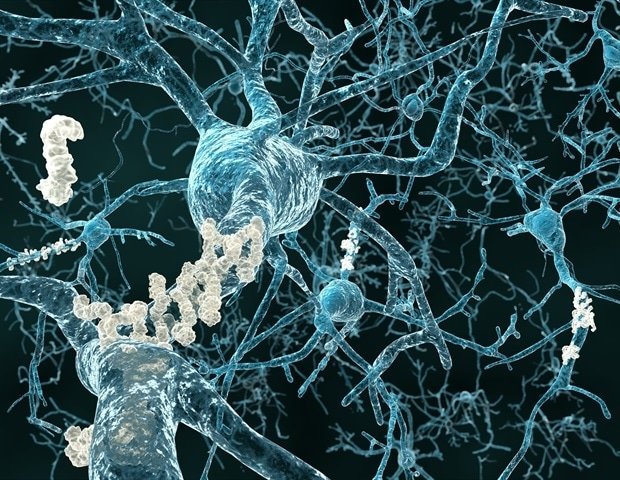
While AD is a uniquely human condition, it can be studied in the laboratory with mice engineered to express genetic mutations that cause AD in humans. The researchers used two of these models. One line of mice carried multiple human mutations in amyloid processing, and the other line of mice carried a human mutation in the tau protein. Amyloid and tau pathology are two of the major early events in AD, and both lines of mice develop AD-like brain pathology, including deterioration of the blood-brain barrier, axonal degeneration, neuroinflammation, impaired hippocampal neurogenesis, impaired synaptic transmission, and extensive accumulation of oxidative damage. These mice also develop severe cognitive impairments that resemble what is seen in people with AD.
Since we found that NAD+ Levels in the brain plummeted in both human and mouse AD, the research team examined whether the loss of brain NAD was prevented+ pre-disease balance or restoration of brain NAD+ balance after significant disease progression, could prevent or reverse AD, respectively. The study built on their previous work, published in Proceedings of the National Academy of Sciences of the USA, showing that restoration of brain NAD+ balance achieved pathological and functional recovery after severe, long-term traumatic brain injury. They restored the NAD+ balance by administering a now well-characterized pharmacological agent, known as P7C3-A20, developed in the Pieper lab.
Notably, not only NAD retention+ The balance protected the mice from developing AD, but delayed treatment in mice with advanced disease also allowed the brain to correct the major pathological events caused by the genetic mutations. Furthermore, both lines of mice fully recovered cognitive function. This was accompanied by normalized blood levels of phosphorylated tau 217, a newly approved clinical biomarker of AD in humans, providing confirmation of disease reversal and highlighting a potential biomarker for future clinical trials.
“We were very excited and encouraged by our results,” said Andrew A. Pieper, MD, PhD, senior study author and director of the Brain Health Medicines Center, Harrington Discovery Institute at UH. “Restoring the brain’s energy balance achieved pathological and functional recovery in both lines of mice with advanced Alzheimer’s. Seeing this effect in two very different animal models, each from different genetic causes, reinforces the idea that restoring the brain’s NAD+ balance can help patients recover from Alzheimer’s.”
Dr. Pieper also holds the Morley-Mather Chair in Neuropsychiatry at UH and the CWRU Rebecca E. Barchas, MD, DLFAPA, University Professor in Translational Psychiatry. He serves as a Psychiatrist and Investigator at the Louis Stokes VA Geriatric Research Training and Clinical Center (GRECC).
The results prompt a paradigm shift in how researchers, clinicians, and patients may think about treating AD in the future. “The key is a message of hope – the effects of Alzheimer’s may not inevitably be permanent,” said Dr Pieper. “The damaged brain can, under certain conditions, be repaired and regain its function.”
Dr. Chaubey further explained, “Through our study, we have demonstrated a drug-based way to achieve this in animal models, and we have also identified candidate proteins in the human AD brain that may be associated with the ability to reverse AD.”
Dr. Pieper emphasized that NAD is currently available over the counter+-Precursors have been shown in animal models to increase cellular NAD+ at dangerously high levels that promote cancer The approach in this study, however, uses a pharmacological agent (P7C3-A20) that allows cells to maintain the correct balance of NAD+ under conditions of otherwise excessive stress, without elevation of NAD+ at supranormal levels.
“This is important when considering patient care, and clinicians should consider the possibility that therapeutic strategies aimed at restoring the brain’s energy balance may offer a pathway to disease reversal,” said Dr. Pieper.
This work is also encouraging new research into complementary approaches and potential trials in patients, and the technology is being commercialized by Glengary Brain Health, a Cleveland-based company co-founded by Dr. Pieper.
“This new therapeutic approach to recovery needs to be translated into carefully designed human clinical trials to determine whether the efficacy seen in animal models translates to human patients,” explained Dr. Pieper. “Additional next steps for laboratory research include identifying the aspects of the brain’s energy balance that are most important for recovery, identifying and evaluating complementary approaches to reversing Alzheimer’s, and investigating whether this recovery approach is also effective in other forms of chronic age-related neurodegenerative disease.”
Source:
Journal Reference:
Kalyani et al. “Pharmacological reversal of Alzheimer’s disease in mice reveals potential therapeutic nodes in the human brain”. Cell Reports Medicine. DOI: 10.1016/j.xcrm.2025.102535