Do you have prostate cancer? The answer to this question is usually a multi -step process, with each step bringing another key element to the puzzle.
Step 1 is the PSA View Test, which may or may not be accompanied by a rectum test (we can name this step 1A.) The problem with the rectum examination is that it rarely fishing cancer already by PSA blood test. This is due to the fact that it takes a while for prostate cancer to reach the point of being visible (capable of feeling from a doctor’s finger). Rectum examination was the most important way in which prostate cancer was diagnosed, but today the PSA trial offers The gift of time: It can detect prostate cancer years earlier than rectum examination. So let’s put the rectum exam, well, behind us for now, and focus on what to do after you have an increased PSA. (For what your PSA number should be for your age, please see this post.) Your doctor may order a PSA repetition, and if it is increased or if the PSA has increased by more than 0.75 ng/ml (see this PSA speed post) in one year, then:
Step 2 is … Prostate Biopsy? No! As we discussed on this site and in book, A biopsy is invasive, is expensive and there is a risk of infection if you have the permeable approach (instead of the best and modern transplay, discussed here). Also, if you have the standard TRUS biopsy (transrestal Olderiond), prostate cancer is more likely to lose. The ultrasound is not just as good as magnetic resonance imaging in the appearance of suspicious areas in the prostate. A Fusion MRI biopsy combines two forms of imaging (MRI and ultrasound) to get a better image. Here is a fun fact: each needle core of a prostate biopsy samples only 1/10,000th prostatic! As I said in the book, it’s like looking for with A needle on the haystack. Thus, doctors need all the help they can reach to target suspicious prostate areas.
But we are not yet ready to pull the trigger in the biopsy. We need more information. Step 2 is a second -line blood or urine testsuch as a 4K score test or PHI test (prostate health index), discussed here. These tests are looking for cancer biomarkers and are designed to answer this question: Is my increased PSA coming from clinically significant cancer – the species to be treated – or comes from BPH, benign prostate enlargement?
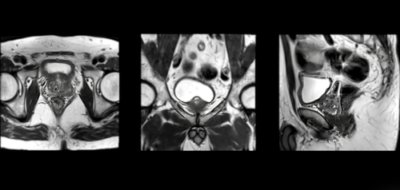
If the second -line test indicates clinically significant cancerthen Step 3 is … biopsy? No! Is a prostate magnetic resonance imaging. As mentioned above, magnetic resonance imaging can find cancer that loses that the ultrasound. Just look at the story of this man. Until its cancer is diagnosed, after several years from a growing PSA and without answers, it had a scar tissue within the prostate from multiple vague TRUS biopsies, including satiety biopsies. The poor protector of man was a pincushion. Then he got a magnetic resonance imaging, which was found a suspicious area of his patron. The man underwent MRI fusion biopsy, his cancer was found, had surgery and at the age of 48 he was without cancer.
So this is step 3: prostate mriand as a landmark of 2018 ACCURACY The study showed that the use of magnetic resonance imaging before biopsy and biopsy aimed at magnetic resonance imaging is “superior to typical biopsy guided by ultrasound in men in clinical risk for prostate cancer”. In the study, clinically significant cancer was found in 38 % of men in the biopsy group aimed at magnetic resonance imaging compared to 26 % of the standard TRUS biopsy group. Another bonus: Only 9 % of men in the biopsy group aimed at magnetic resonance imaging has proven to have clinically insignificant cancer (who will not need treatment immediately and may never need it), unlike 22 % of men in the standard biopsy group.
Step 4 is biopsyBut we will stay in step 3 for now.
The score pi-rads
A prostate damage is not always caused by cancer. Infection or BPH Can cause suspicious areas in the prostate. Thus, radiologists have ended up in PI-RADS Sort ScaleHe appreciates how likely it is that a man with damage has prostate cancer. The Pi-Rads scale goes from 1 to 5. Score 1 or 2 means that there is no suspicious harm or that the findings are consistent with BPH.*
*Let’s put a pin on it, no biopsy is intended. We will return to low Pi-Rads scores in a minute.
PI-RADS Rating 3 It means that there is an intermediate risk of prostate cancer, and this should cause biopsy.
PI-RADS rating 4 or 5 It means that the damage has a high or very high risk of being cancer.
The lower the Pi-Rads rating, the greater the chance of having no biopsy cancer or if you do, it will be insignificant. The higher the Pi-Rads rating, the greater the chance of having significant cancer to be treated. Using data from the precision test, your chances of having significant cancer found are: 12 % if you have PI-RADS 3. 60 percent if you have PI-RADS 4? and 83 percent if your Pi-Rads are 5.
So: If my pi-rads are 1 or 2, am I from the hook? Not necessarily. Like Any diagnostic test for prostate cancerMagnetic resonance imaging is not perfect and low-grade cancer-alterations containing only the Gleason 3 (for 3 + 3 = 6 or Grade 1 group)-often do not appear. This is due to the fact that these slowly growing prostate cancer cells do not obviously look different compared to the normal prostate cells.
Here is where the PSA density can help provide clarity. PSA density is the PSA score divided by prostate volume (specified by TRUS or MRI). The lower your PSA density (lower than 0.1), the lower the risk of having prostate cancer. If your PSA density is higher than 0.15, you have a higher risk of being diagnosed with group 2 (Gleason 7) or higher cancer. Even this may not have to be treated immediately.
Here is a free note for magnetic resonance imaging: I had a magnetic resonance imaging to look at a tendon on my thumb and learned that I am Really, really claustrophobic. It was an older machine, incredibly loud, and the technicians who did the test were playing this terrible music in the tube with multiple words F. I couldn’t think, I couldn’t pray consistently or form two sentences together on my head because of this. For some reason, they couldn’t get a good picture and it took almost 90 minutes. I got through it, but it was one of the worst, most things that cause panic I ever did. If you are claustrophobic, talk to your doctor! It may be possible to go first to the feet of the machine, which would be great – at least your head would not be in the tube. It may be that your magnetic resonance imaging is one of the younger generations, which is less like a torpedo tube and are, blessed, more open. Or, like Weill Cornell Medical Urologist Jim Hu, MD, MPH, who provided expert opinion on the diagnosis and staging chapter at book, Suggested, your doctor may prescribe a Baltic to help you relax there. There is no shame: If you need it, you need it.
In addition to the book, I have written about this story and much more about prostate cancer on the prostate cancer website, Pcf.org. The stories I wrote are under the categories, “understanding prostate cancer” and “for patients”. As we have said for years Patrick Walsh; Knowledge is power: Saving your life can start with the transition to the doctor and know the right questions you need to ask. I hope all men put prostate cancer on their radar. Take a basic PSA blood test in the early 1940s and if you are African descent or if the cancer and/or prostate cancer runs to your family, you should regularly examine for the disease. Many doctors do not do this, so it is up to you to ask for it. NOTE: I am a subsidiary of Amazon, so if you click on the link and buy a book, I will theoretically make a small amount of money.
© Janet Farrar Worthington