The study funded by NIMH used universal examination, risk assessment and safety planning to reduce suicide attempts among patients with pre -instalculation patients
• Investigation
Suicide is a leading cause of death in the United States and major public health concerns. Previous research has shown that the identification and help of people who are at risk of suicide during regular care visits can help prevent it. Primary care clinics are particularly important in this respect, as the research has shown 40% of people who died of suicide appeared in this environment in the month before their death.
A recent study funded by the National Institute of Mental Health (NIMH) found that when primary care clinics added suicide care practices to usual visits, suicide efforts decreased by 25% in 3 months after visit. The findings emphasize how detrimental it may be for primary care clinics to take an active role in preventing suicide and help strengthen health systems to integrate these practices into clinical care.
What did the researchers do in the study?
Clinicians of primary care for depression during most care visits and depression often include questions about the risk of suicide. Before Research supported by Nimh He found that the check for suicidal thoughts and behaviors followed by a short security plan may reduce the risk of suicide efforts.
Researchers Julie Angerhofer Richards, Ph.D., mph At the Kaiser Permanente Washington Health Research Research Institute, it aims to find out whether the incorporation of suicide care into normal adult primary care visits could prevent subsequent suicide attempts.
This study analyzed the secondary data from a greater comprehensive study of National zero suicide model . The integrated zero suicide approach is the first US program associated with a significant reduction in suicides among patients with health behavior. The research team previously examined this model in a Separate study funded by Nimh in six health systems in all the United States.
Prior to intervention, providers handed care as usual, which did not include suicide or population monitoring. The 22 participating clinics were randomly commissioned to start providing suicide care on gradual dates (4 months away) for a period of 2 years. During the study, 333,593 patients were observed for over 1.5 million primary care visits.
Suicide Care consists of:
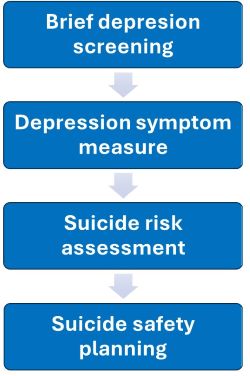
- Depression Check: All patients have completed a brief two -question screening screening, followed by a larger scale of depression symptoms for those who have made a positive question.
- Scale of Symptoms of Depression: Screner was followed by a larger scale of depression symptoms for patients who posed positively to each question.
- Suicide Risk Assessment: Patients with thoughts of self -injury or suicide completed a measure of suicidal thoughts and behaviors.
- Suicide Safety Planning: Patients who reported intention or suicide plans last month were referred to the specified personnel, including social health workers, to plan a suicide safety of the same day. Security planning was a collaborative process between patients and providers involving the identification of warning signs, registration of strategies and treatment supports and the creation of safe environments to manage a suicide crisis.
Three basic strategies supported intervention:
- Specialists have led to each clinic and met with staff on a continuous basis to provide support and problem solving.
- The support of clinical decisions, including reminders prior to the visit and prompt prompts, came from the electronic medical system of clinics.
- Regular monitoring of the performance of medical records reported on clinics for control and evaluation.
The researchers compared clinics that provide suicide care to clinics that provide usual care for:
- Benefits to document the suicide risk and safety planning in the medical record within 2 weeks of the Primary Care Visit at risk
- Percentages of suicide or death of patients with suicide at 90 days after their visit to their primary care
What did the results of the study show?
The integration of suicide care into regular primary care visits led to significantly higher rates of sorting, evaluation and planning of collaborative security. The intervention in turn led to a 25% reduction in suicide efforts to 90 days after a primary care visit compared to the usual clinical care. Together, the results show that the incorporation of suicide prevention practices into adult primary care leads to more people who are shown for suicidal thoughts and behaviors and fewer suicide attempts once they leave the clinic.
These findings support The hierarchy of prevention of Nimh’s suicide prevention in healthcare arrangements with the ultimate goal of reducing the suicide rate in the United States. The study provides the critical next steps for providers and care groups that respond to suicidal concerns during clinical practice, helping to rescue lives in the process.
Reference
Richards, Ja, Cruz, M., Stewart, C., Lee, Ak, Ryan, TC, Ahmedani, BK, & Simon, GE (2024). Effectiveness of incorporating suicide care in primary care: Secondary analysis of a pace, randomized application test. Annals of Internal Medicine; 177(11), 1471-1482. https://doi.org/10.7326/m24-0024
Financing
If you or someone you know is struggling or having suicide thoughts, call or send text to suicide and life of crisis 988 988 or chat to 988lifeline.org . In life -threatening situations, call 911.
For more information on suicide prevention, see:
Refusal
The zero suicide framework was developed at the Education Development Center (EDC) through the Center for Suicide Prevention Resources funded by federal funding and the National Action Alliance to prevent suicide. Zero suicide information and brand is freely available in zero suicide ToolboxSm governed by EDC. No official approval by EDC is intended or must be inferred.
