NIMH-funded study used universal screening, risk assessment and safety planning to reduce suicide attempts among adult primary care patients
• Research Highlights
Suicide is the leading cause of death in the United States and a major public health concern. Previous research has shown that identifying and helping people at risk of suicide during regular care visits can help prevent it. Primary care clinics are particularly important in this regard, as research has shown that beyond 40% of people who died by suicide seen in this setting the month before their deaths.
A recent study funded by the National Institute of Mental Health (NIMH) found that when primary care clinics added suicide drills to routine visits, suicide attempts decreased by 25% at 3 months after the visit. The findings highlight how important it can be for primary care clinics to take an active role in suicide prevention and help health systems integrate these practices into clinical care.
What did the researchers do in the study?
Primary care clinicians screen for depression during most care visits, and depression screeners often include questions about suicide risk. Before Research supported by NIMH found that screening for suicidal thoughts and behaviors followed by brief safety planning can reduce the risk of suicide attempt.
Researchers led by Julie Angerhofer Richards, Ph.D., MPH at the Kaiser Permanente Institute for Health Research in Washington, D.C. aimed to see if incorporating suicide care into routine adult primary care visits could prevent subsequent suicide attempts.
This study analyzed secondary data from a larger comprehensive study of National zero-suicide model . The Zero Suicide Comprehensive Approach is the first US program linked to a significant reduction in suicide among behavioral health patients. The research team previously tested this model in a separate NIMH-sponsored study in six health systems in the United States.
Before the intervention, providers provided care as usual, which did not include population-based suicide screening or follow-up. The 22 participating clinics were randomly assigned to begin providing suicide care at staggered dates (4 months apart) over a 2-year period. During the study, 333,593 patients had more than 1.5 million primary care visits.
Suicidality care consisted of:
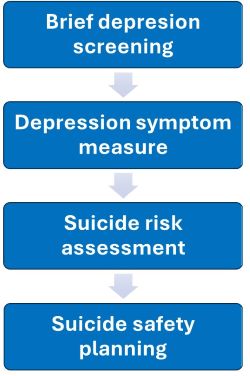
- Depression Check: All patients completed a short two-question depression screening, followed by a longer depression symptom scale for those who scored positively on each question.
- Depression Symptom Scale: Screening was followed by a longer depression symptom scale for patients who scored positively on each question.
- Suicide Risk Assessment: Patients with self-harm or suicidal thoughts completed a measure of suicidal thoughts and behaviors.
- Suicide Safety Planning: Patients who reported suicidal intent or plans in the past month were referred to designated care staff, including mental health social workers, for same-day suicide safety planning. Safety planning was a collaborative process between patients and providers that included identifying warning signs, documenting coping and support strategies, and creating safe environments for managing a suicidal crisis.
Three main strategies supported the intervention:
- Skilled facilitators led trainings at each clinic and met with staff on an ongoing basis to provide support and resolve issues.
- Clinical decision support, including pre-visit reminders and visit prompts, came from the clinics’ electronic medical record system.
- Regular monitoring of medical record performance reported in clinician review and assessment rates.
Researchers compared clinics providing suicide care with clinics providing usual care in:
- Rates of providers documenting suicide risk assessment and safety planning in the medical record within 2 weeks of an at-risk patient’s primary care visit
- Rates of suicide attempt or death by suicide of patients in the 90 days following their primary care visit
What did the study results show?
Incorporating suicide care into routine adult primary care visits resulted in significantly higher rates of suicide risk screening, assessment, and collaborative safety planning. The intervention in turn led to a 25% reduction in suicide attempts in the 90 days following the primary care visit compared to usual care clinics. Together, the results demonstrate that incorporating suicide prevention practices into adult primary care results in more people being screened for suicidal thoughts and behaviors and fewer suicide attempts once they leave the clinic.
These findings support The NIMH priority for suicide prevention in health care settings with the ultimate goal of reducing the suicide rate in the USA. The study provides critical next steps for providers and care teams to respond to suicidal concerns during clinical practice, helping to save lives in the process.
Reference
Richards, JA, Cruz, M., Stewart, C., Lee, AK, Ryan, TC, Ahmedani, BK, & Simon, GE (2024). Effectiveness of integrating suicide care into primary care: Secondary analysis of a cluster-randomized implementation trial. Annals of Internal Medicine, 177(11), 1471–1482. https://doi.org/10.7326/M24-0024
Financing
If you or someone you know is struggling or having suicidal thoughts, call or text the 988 Suicide and Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911.
For more information on suicide prevention, see:
Refusal
The Zero Suicide Framework was developed at the Education Development Center (EDC) through the federally funded Suicide Prevention Resource Center and the National Suicide Prevention Lifeline. The Zero Suicide brand and information are freely available on Zero Suicide ToolboxSM managed by EDC. No official endorsement by EDC is intended or should be inferred.
