A landmark review reveals how your mouth germs shape the health of the bowel, immunity and chronic illness, making oral care a first -line strategy for the prosperity of the whole body.
Review: The oral microbial axis throughout life: new ideas for a forgotten interaction. Credit Picture: Shutterstock
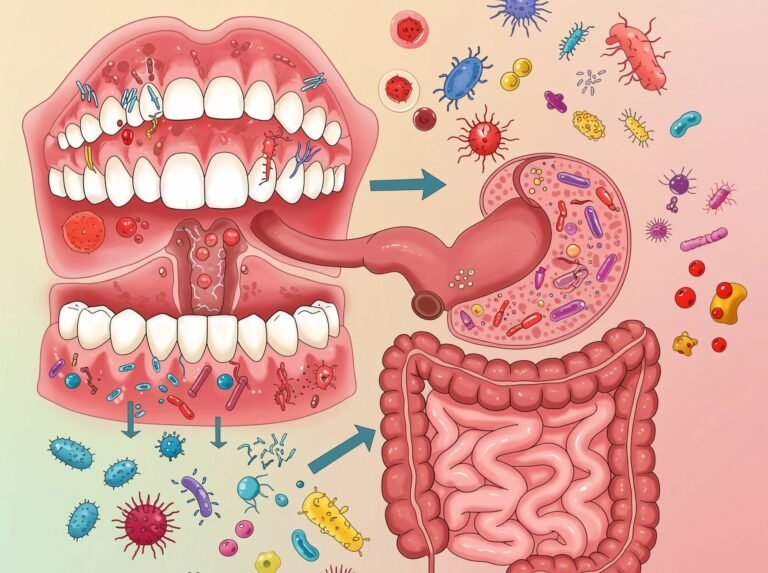
In a recent study in the magazine NutrientsThe researchers have collected and compose nearly 250 publications that explore the “oral axis”, a complex, two -way communication network connecting the gut germicide and the much less thoughtful copy of the oral (oral microbicide).
The review findings emphasize that oral pathogens can migrate to the intestine, cause difficulty and contribute to systemic diseases such as inflammatory bowel disease (IBD), colon cancer and cardiovascular disease (CVDs). This disorder is mediated by direct bacterial displacement and by various microbial metabolites, including trimethylamine N-oxide (TMAO) and special lipopolysaccharide (LPS), as well as other metabolite such as fatty acids.
The review also emphasizes the importance of beneficial ordinary germs and dietary agents, such as fibers, polyphenols and probiotics, in maintaining a healthy oral-gaz. Maintaining oral health is a critical, but often forgotten, component of overall systematic prosperity.
Why the mouth is important
The microbicide studied extensively has been welcomed for more than a decade as a major regulator of human health, affecting everything from immune function and metabolism to neurology and mood. However, science has largely ignored that the digestive tract that culminates in the gut begins in the mouth.
Specifically, a handful of studies investigating the gut microbial synthesize that the oral cavity hosts its own separate and complex microbial community of over 700 microbial species. Even when studied, the oral microbicide has been studied is studied individually and focuses more on the prevention of bowel disease and cavities rather than digestion and immunity.
Recent research suggests the existence of two -way dialogue between oral and bowel microflora, with potentially deep impact on holistic well -being.
In addition, disorders either in microbicide, especially in different stages of life, such as infancy, aging or during chronic diseases, can affect the other, underlining a perspective of life in the interactions of the mouth.
Four communication routes
This narrative review composes the consistently developing body of evidence that explores the “axis of the oral-brilliant”, with the aim of clarifying the mechanisms through which these separate microbial communities interact and how these interactions influence human health.
It covers nearly 250 studies throughout microbiology, gastroenterology and systemic medicine, focusing on literature describing any of the three primary communication pathways connecting the microbial and microbes of the mouth: the intestinal pathway, which is the immediate transport. The hematogenic pathway, which is the spread of germs through blood circulation. and the mediation of metabolite, which includes the systematic effects of chemical compounds produced by both microbes.
In addition, the review describes a fourth path, the stool course, where bowel germs can reach the mouth, especially in poor hygiene or sewer arrangements, further supporting a two -way communication model.
The review examines and synthesizes details on each path, thereby presenting a coherent picture of how oral difficulty (an imbalance in the mouths in the mouth) can directly affect bowel health and cause systemic diseases, while underlines potential protective strategies.
The intestinal route
The extensive set of literature revises the most important that the relationship between the mouth and the intestine is dynamic, multifaceted and much more interconnected than it is commonly believed.
People swallow 1 to 1.5 liters of saliva daily, which serve as a pipeline for billions of bacteria. While most are killed by stomach acid, some resistant pathogens can survive, especially in people with weakened defenses, such as those using proton pump inhibitors.
ALWAYS ALWAYS Gingivalis porphyromonas and Nucletius fusobacteriumBoth key players in the periodontal (gum) disease have been colonized that they colonize the intestine and are strongly involved in driving chronic diseases associated with inflammation such as inflammatory bowel disease (IBD).
The review notes that some oral germs, such as Projector Species can also be detected on stools under normal normal conditions. With concern, these oral germs have been associated with promoting the growth of colon tumors.
The bloodthirsty route
While it is significantly more difficult to invade, blood circulation has a much more threatening pathway for oral bacteria in systematic circulation from the digestive tract. Poor oral health, especially periodontitis, creates inflammatory, progressive gums that serve as an immediate entry point for oral bacteria to invade the circulatory system.
This “oral bacteremia” allows pathogens to travel to remote organs, including the intestine, where they can disrupt the intestinal barrier, causing the “bowel leakage” syndrome and cause systemic inflammation. This can, in turn, activate a waterfall where the pathogenic bowel bacteria can then use this bowel leak to invade blood circulation, creating a completely independent set of infections.
Studies in animals and human Nucletius fusobacteriumwhich are associated with both intestinal inflammation and colon cancer.
Oral bacteria in circulation can also aggravate systemic inflammation, metabolic disorders and even affect the synthesis of guts.
Communication with metabolite mediation
Interactions with metabolite mediation are the most complex oral interactions. Both cogs, oral microbes and intestines, produce a diverse and largely independent range of bioactive compounds. The trimethylamine n-oxide (TMAO), a metabolite strongly associated with atherosclerosis, is perhaps the best studied.
Specifically, TMAO is produced in a two -stage process where intestinal bacteria first convert dietary nutrients such as choline and carnitine from red meat and eggs into trimethylamine (TMA), which the hepatic enzyme containing flavine monoxygenase (FMO3) is then converted.
Alarmingly, oral pathogens such as P. Gingivalis It can aggravate this process by increasing systematic inflammation, which in turn stimulates FMO3 expression and increases the TMAO levels in turn, severely increasing the risk of atherosclerosis.
The review further details that other metabolites, including short -chain fatty acids (SCFAS), Indol and its derivatives and altered bile acids, play critical roles in regulating inflammation, immunoocials, integrity and integrity. For example, butyric, a SCFA produced in the intestine, can have both anti -inflammatory and metabolic effects. Indol derivatives can protect the bowel barrier and regulate immune balance.
The balance of these metabolites is influenced by both the health of the microbial and the intestine and the dietary standards.
The course of the stools
The review emphasizes the importance of the fecal road, especially in poor drainage or immunosuppressed situations. Germs from the intestine can reach the oral cavity through contaminated foods, water or direct contact, affecting both oral and bowel health.
This pathway is also related to the spread of certain viruses and gastrointestinal diseases.
Incorporating bowel oral and health
This review underlines the strong interconnection between the microbial and the microbes of the oral and intestinal and the importance of increasing research that focuses on the disease and digestion in the oral bacteria.
Our oral and microbial microbials are not isolated ecosystems, but they are deep interconnected parts of a larger set. The health of our mouths directly affects the health of our bowel and vice versa, with profound effects on systemic health and clinical intervention.
The review emphasizes that dietary patterns, including high intake of dietary fibers, polyphenols, omega-3 fatty acids, prebiotics and probiotics, can support both the microbial balance of the oral and the intestine, while the malnutrition, while Therefore, preventive strategies should aim at both oral and intestinal health during life.
The data are increasing, but many of the detailed mechanisms remain under investigation, underlining the need for continuing interdisciplinary research.
Magazine report:
- Azzolino, D., Carnevale-Schianca, M., Santacroce, L., Colella, M., Felicetti, A., Terranova, L., Castrejón-Pérez, RC, Garcia-Godoy, F., Lucchi, T. & Passarelli, PC (2025). The oral microbial axis -flowing during life: new knowledge in a forgotten interaction. Nutrients17 (15), 2538. DOI – 10.3390/NU17152538.