A breakthrough treatment targeting disturbing and distressing mental images for people with psychosis could lead to a transformative intervention for a condition estimated to cost England nearly £12 billion a year.
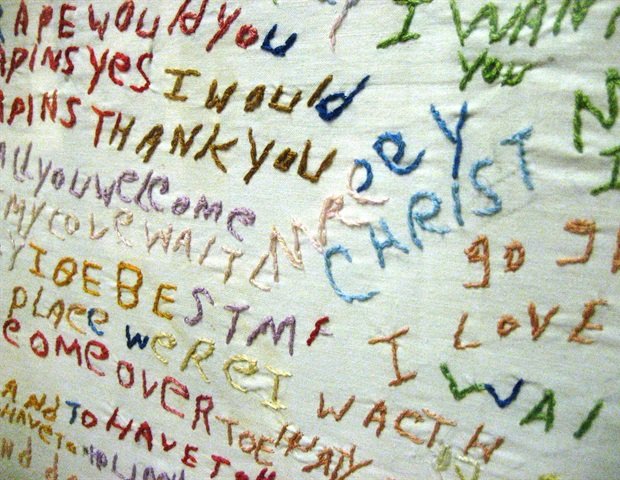
74 percent of people with psychosis, a condition that causes people to hear voices, unfounded fears that others are harming them, also see disturbing images in their mind’s eye. These images can be the result of trauma, stress, fear of anticipated future events, and many other factors.
A recent survey of over 10,000 UK adults found that imagery was the third most strongly linked factor to distrust and paranoia. These vivid images can often be multisensory and associated with disturbing voices, as well as unfounded beliefs that others mean them harm.
Existing psychological treatments, such as Cognitive Behavioral Therapy (CBT), have shown a strong but small effect in treating psychotic experiences such as hallucinations and delusions. Similarly, while antipsychotic medications can relieve some psychotic symptoms, about 74 percent of patients stop or switch medications within 18 months. This is largely due to debilitating side effects or a lack of reported benefit, highlighting the critical need for more effective treatments.
The University of Sheffield research team believe that imagery-focused therapy could be a valuable intervention to complement existing treatments.
iMAPS therapy aims to directly address such images with the “mind’s eye” by helping the patient to understand, understand and change the images, replacing them with more positive ones. It also targets negative beliefs about self and others (schemas) using imagery techniques. A trial funded by the National Institute for Health and Care Research (NIHR) recruited 45 patients with psychosis who were seeking help with hallucinations and delusions and had reported distressing and distressing mental images associated with their symptoms.
The largest feasibility trial to date of imagery-focused therapy for people with psychosis with 45 patients, detailed in a University of Sheffield study recently published in the journal Schizophrenia Bulletin, demonstrated the safety of iMAPS and yielded promising results, leading to hopes for a multicenter clinical trial to test the treatment’s clinical and economic effectiveness.
Imagine someone experiencing psychosis who has the terrifying belief that their home is about to be invaded and attacked. They could then vividly imagine an intruder breaking in, causing intense fear and exacerbating their anxiety.”
Dr Christopher Taylor, Senior Lecturer and NIHR Fellow, School of Psychology, University of Sheffield
Dr. Taylor is also Consultant Clinical Psychologist, Pennine Care NHS Foundation Trust.
He added, “This intrusive image can reinforce their suspicion and paranoia, making them feel even more vulnerable. Our goal is to help them understand and ultimately gain control over these powerful images. When you try to suppress disturbing mental images, they often come back more strongly—like the New Year’s resolution to avoid the chocolate chip cookie.”
“In therapy, we address this by helping people make sense of these shared experiences. We gently introduce imagery work with ‘safe place’ exercises to cultivate feelings of safety, and then practice changing the size, shape and texture of the image to build a sense of control. We also use imagery rewriting, a technique borrowed from trauma therapy, while guiding people to imagine a positive event. We cannot change the past, we can empower individuals to rewrite their experiences and change meaning.’
In the trial, speech therapy was administered in 12 weekly sessions. each patient had at least one unpleasant image associated with a hallucination or delusion. These may also include purely imaginary images along with those from a person’s past or future concerns.
Thom Brandwood-Spencer, 28, who took part in the first iMAPS study, started experiencing painful symptoms when he was about nine years old.
“It first manifested as a general fear, where I would walk home from school and jump from lamppost to lamppost to avoid this abstract fear. When I was 12 or 13, I started hearing disturbing voices and a year later, I started seeing things, which evolved into eerie, featureless figures making strange noises.
“It was very painful and difficult to understand. I often felt that I was in danger, as if the sights and sounds were portents of things to come.”
Thom was later referred to local mental health services and eventually diagnosed with paranoid schizophrenia with psychotic episodes. Through support, his condition became more manageable and he went on to study IT at university – but his visions continued to fill him with terror and paranoia and eventually forced him to drop out.
It was at that point, while under the care of a first-episode psychosis team, that Thom engaged with iMAPS, and over eight weekly sessions, his therapist helped him understand and change the narrative of the images he was experiencing.
“At that point, the condition was completely tearing my life apart and the prescription drugs I was taking weren’t working,” she said.
“One of the most difficult aspects was helplessness – and the idea that what was happening to me was permanent and inevitable. iMAPS helped me deal with this by changing this narrative of helplessness and understanding that my life and experiences are not predetermined. The therapy enabled me to shift my focus away from what I was seeing in my mind.
“I realized that the threat didn’t come from the figures, but from my own feelings, and I realized that made a big difference. We also used a technique to imagine putting the hapless figures in a suit of armor or a diving suit, and it helped me feel like I couldn’t be caught anymore.”
Thom successfully completed an undergraduate degree in Psychology and then went on to pursue a Masters in the same field. He now works in a role supporting others with mental health issues and even discussed his experiences with iMAPS at an international conference.
“As well as the benefits of the iMAPS treatment itself, I was able to act as a consultant in the latest study and as an advocate to help others going through similar experiences. Now I can give people what I needed when it all started.
“One of the most important messages I would like to pass on to others is that whatever you’re going through, it doesn’t have to be forever. It can change and there is hope.”
Dr Taylor from the University of Sheffield added: “We are very encouraged by the feedback from patients like Thom, who serves as a great advocate not only for iMAPS but also for recovery and supporting others with similar experiences.
“A full clinical trial is the necessary next step to assess the wider clinical and cost-effectiveness of iMAPS, paving the way for it to potentially complement the offer of existing NICE-recommended psychosis treatments.”
Source:
Journal Reference:
Taylor, CDJ, et al. (2025). IMagery Focused Therapy for PSychosis (iMAPS-2): An Assessor-blind Feasibility Randomized Controlled Clinical Trial. Schizophrenia Bulletin. doi.org/10.1093/schbul/sbaf060.