In a recent study published in the journal Nature, Researchers in the United States of America designed and discovered lolamycin, a selective antibiotic that targets the lipoprotein transport system in Gram-negative bacteria. They found that lolamycin was effective against multidrug-resistant Gram-negative pathogens, showed efficacy in mouse models of infection, spared the gut microbiome, and prevented secondary infections.
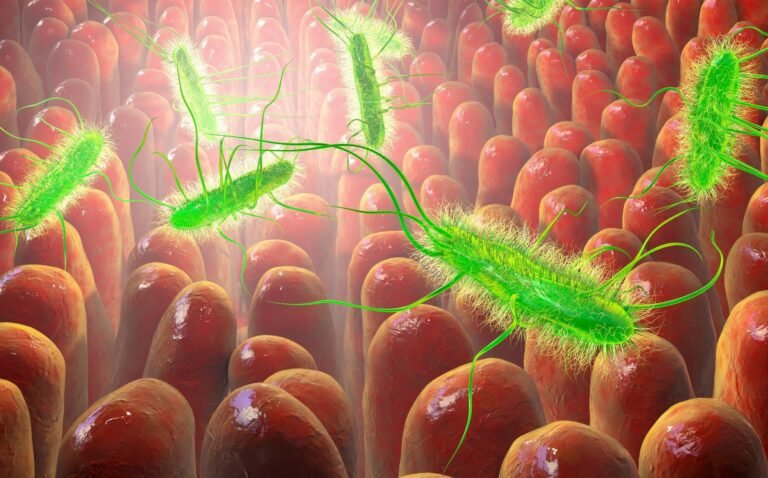
Study: A Gram-negative-selective antibiotic that protects the gut microbiome. Image Credit: Katerina Kon / Shutterstock
Record
Antibiotic treatment can disrupt the gut microbiome, leading to increased susceptibility to pathogens such as C. difficile and higher risks of gastrointestinal, kidney, and blood problems. Most antibiotics, whether gram-positive only or broad-spectrum, damage the intestinal organs and cause dysbiosis. The impact of Gram-negative-only antibiotics on the microbiome is unclear due to the rarity of such compounds. Their discovery was challenging because most antibiotic targets are shared by both Gram-positive and Gram-negative bacteria. Since the gut microbiome contains many Gram-negative bacteria, indiscriminate Gram-negative antibiotics such as colistin can cause significant dysbiosis, limiting their use.
Despite the growing need for new Gram-negative antibacterial agents due to resistant infections, no new class has been approved by the Food and Drug Administration (FDA) for more than 50 years. The discovery is complicated by the complex membrane structures and efflux pumps of Gram-negative bacteria. Development of a microbiome-sparing Gram-negative-only antibiotic requires targeting a key protein exclusive to Gram-negative bacteria, with significant homology differences between pathogenic and commensal bacteria. In the present study, the researchers designed and reported a single Gram-negative antibiotic called “lolamycin”, which targets the Lol lipoprotein transport system in the periplasm, which is crucial for various Gram-negative pathogens.
About the study
In the present study, LolCDE, a key component of the Lol system in Gram-negative bacteria, was targeted. Potential inhibitors of the system were screened, synthesized and evaluated. The efficacy of lolamycin was evaluated against multiresistant clinical isolates of it E. coli, K. pneumoniae, and E. cloacae. Susceptibility studies were performed with lolamycin and other compounds.
Lolamycin-resistant mutants were developed and compared for fitness. The bactericidal effects of lolamycin were examined using growth-time-kill curves. Confocal microscopy was used to observe phenotypic changes in the target bacteria. Molecular modeling and dynamics simulations, ensemble docking and cluster analysis were used to investigate the binding sites and inhibition mechanism of lolamycin.
Further, mice were treated with pyridinepyrazole (compound 1) and lolamycin intraperitoneally for three days. Pharmacokinetic studies were performed to assess the bioavailability of lolamycin. Infection models were used to compare the efficacy of lolamycin and compound 1 in the treatment of pneumonia and sepsis, with lolamycin also administered orally. Mice microbiomes were analyzed using their stool samples via 16S ribosomal ribonucleic acid (RNA) sequencing. Additionally, antibiotic-treated mice were challenged with C. difficile to assess their ability to clear the pathogen spontaneously.
Results and discussion
Lolamycin, an inhibitor of the LolCDE complex, showed potent activity against specific Gram-negative pathogens with low accumulation in E. coli. Lolamycin showed selectivity, avoiding both Gram-positive and Gram-negative commensal bacteria. It showed minimal toxicity to mammalian cells and remained effective in the presence of human serum. Lolamycin showed potent activity against multiresistant clinical isolates of E. coli, K. pneumoniae, and E. cloacae. Lolamycin outperformed the other compounds, showing a narrow minimum inhibitory concentration range and efficacy against multidrug-resistant strains.
Sequencing of lolCDE in resistant strains revealed no mutations associated with lolamycin resistance, underscoring its potential as a promising antibiotic candidate. Lolamycin showed lower frequencies of resistance among strains. LolC and LolE proteins were identified as targets, with specific mutations associated with resistance. Lolamycin showed bactericidal or bacteriostatic effects against the tested bacteria. Swelling was observed in cells treated with lolamycin, indicative of dysfunctional lipoprotein trafficking. Lolamycin-resistant mutants showed altered phenotypic responses to treatment, supporting the involvement of LolC and LolE.
Lolamycin was found to disrupt lipoprotein trafficking by competitively inhibiting binding to the BS1 and BS2 sites. Hydrophobic interactions were found to primarily drive the binding of lolamycin, explaining the reduced efficacy of compounds with primary amines. Resistance mutations were found to affect the binding affinity of lolamycin, highlighting their role in destabilizing the binding pockets. Lolamycin demonstrated superior efficacy to compound 1 in reducing bacterial load and improving survival rates in infection models involving multidrug-resistant bacteria such as E. coli AR0349, K. pneumoniaeand E. cloacae.
Oral administration of lolamycin showed significant bioavailability and efficacy, reducing bacterial load and increasing survival rates in mice infected with colistin-resistant E. coli. Lolamycin showed minimal effect on gut microbiota with consistent richness and diversity compared to amoxicillin and clindamycin. Lolamycin-treated and vehicle control mice showed minimal C. difficile colonization. In contrast, mice treated with amoxicillin or clindamycin showed an inability to clear C. difficilewith high colonization throughout the experiment.
conclusion
In conclusion, this new study identifies lolamycin as a pathogen-specific antibiotic that holds promise for minimizing damage to the gut microbiome and potentially preventing secondary infections. Further research and human studies are needed to confirm the drug’s clinical application. In the future, lolamycin’s effect on maintaining the microbiome could provide significant advantages over current broad-spectrum antibiotics in clinical practice, enhancing patient outcomes and overall health.
What if there was an antibiotic that didn’t disrupt the gut microbiome?
It exists now.
A discovery has been published @Nature today @PaulHergie and colleagues @UofIllinois @justsaysinmice pic.twitter.com/ONEFWYHEJL— Eric Topol (@EricTopol) May 29, 2024