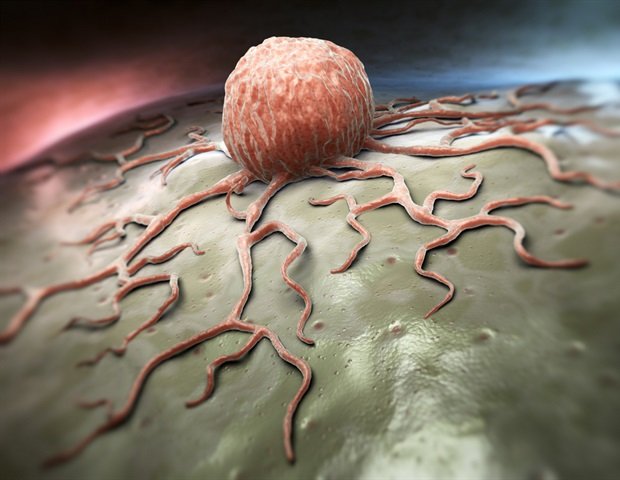
CAR T cells are T cells engineered to attack specific targets found in cancer cells. They have had remarkable results in some blood cancer patients. But they did not perform well against other cancers, including solid-tumor cancers such as pancreatic cancer, prostate cancer and melanoma. Researchers are looking for techniques to enhance the effectiveness of CAR T cell therapy.
The study, published today in Science Immunology, suggests that CD5 knockout could be a key technique. By shedding light on the protein’s previously obscure role, the researchers found that it functions as a powerful immune checkpoint, limiting the effectiveness of T cells. By removing it, they showed that it dramatically enhanced the antitumor activity of CAR T cells in a variety of preclinical cancer models.
We discovered in preclinical models that CD5 deletion significantly enhances CAR T cell function against multiple cancers. The impressive results we observed in preclinical models suggest that CD5 knockout could be a general strategy to improve CAR T cell function.”
Marco Ruella, MD, senior author, assistant professor of Hematology-Oncology, researcher in the Center for Cellular Immunotherapies and scientific director of the Penn Medicine Lymphoma Program
The first author of the study is Ruchi Patel, PhD, a recent graduate student from the Ruella lab.
Key immune checkpoints
Immune checkpoint mechanisms are regulatory switches that help prevent immune responses from becoming too intense and causing collateral tissue damage. Cancers often subvert these mechanisms to suppress antitumor immune responses.
Scientists have already identified several key immune checkpoint proteins, including PD-1 and CTLA-4, which were the targets of early successful immune checkpoint inhibitor therapies, including ipilimumab, nivolumab and pembrolizumab. While researchers are investigating genetic deletion of these proteins to boost CAR T cell therapies, scientists believe there are other, so far unknown immune checkpoint mechanisms that cancers exploit.
Focus strategy on CD5
Before studying the role of CD5 in CAR T cells, researchers initially focused on CD5 as a tumor target. CD5 protein is highly expressed on tumor T cells in T-cell lymphoma and T-cell acute lymphoblastic leukemia, rare blood cancers that have no effective immunotherapy treatment options. Notably, none of the currently available commercial CAR T-cell therapies are approved for the treatment of T-cell lymphomas.
Ruella’s team initially engineered CAR T cells that target CD5-bearing cells to treat these malignancies, but soon realized they needed to delete CD5 on the CAR T cells to prevent the CAR T cells from killing each other , as CAR T cells naturally express CD5. Therefore, using CRISPR-Cas9 technology, they deleted the CD5 gene in the CAR T cells so that the modified cells would not attack each other. This knockout of CD5 in CAR T cells was shown to provide a dramatic boost in their efficacy in laboratory experiments with a variety of T-cell malignancies.
However, researchers soon realized that CD5 deletion was able to broadly enhance the antitumor effect of multiple CAR T products for both solid and liquid cancers. The researchers found similar improvements in efficacy in laboratory studies when they tested the CD5-knockout strategy on CAR T cells designed to target other non-CD5-bearing cancers, such as B-cell leukemias and lymphomas, pancreatic cancer and prostate cancer. They observed increases in CAR T cell proliferation and survival as well as increased tumor cell killing activity, and these results exceeded those seen after knocking out the known immune checkpoint protein PD-1. The researchers also found that knocking out CD5 could improve the antitumor activity of other T cells, again suggesting that CD5 is an important immune checkpoint protein in these cells.
In the study, the team examined the molecular mechanisms of the CD5 knockout, showing that it enhances the activities of genes associated with T cell activation and cell killing efficiency. Analyzing a large database of tumor biopsies, the researchers also linked relatively low CD5 expression on T cells with better patient outcomes.
The research is progressing to clinical trials
A Phase I clinical trial of CD5-knockout CAR T cells will soon begin to enroll patients with CD5-bearing T-cell lymphomas. “If the CD5-knockout strategy is safe and effective in such trials, it could be tested against a wider range of cancers,” Ruella said. “We are excited to see this work move ‘from bench to bedside.’
For more information about cancer clinical trials at Penn Medicine, visit the Abramson Cancer Center Clinical Trials Information Service website or call 1-855-216-0098 to speak with a clinical trial navigator.
The research was supported by funding from the National Institutes of Health and National Cancer Institute (R37-CA-262362-02), the Leukemia and Lymphoma Society, Gilead Research Scholar Award in Hematology, Emerson Collective, Laffey McHugh Foundation, Parker Institute for Cancer Immunotherapy, Berman and Maguire Funds for Lymphoma Research at Penn, American Society of Hematology, and viTToria Biotherapeutics.
Source:
Journal Reference:
Patel, RP, et al. (2024) CD5 Deletion Enhances Antitumor Activity of Positive T Cell Therapies. Science Immunology. doi.org/10.1126/sciimmunol.adn6509.