Maria called with a question, “My baby is 4 weeks old, and my husband and I love her to death. However, she is A lot of work, and we don’t want another small one yet. My husband and I also hope to continue our sex life, but can I be in birth control while breastfeeding? ”
Mothertobaby is here to help answer some of these questions! Of course, before you decide, it is best to talk to your medical provider and receive their tips. Since everyone is different, some birth control methods may not be a good match for you.
Can breastfeeding be used as contraception?
There are many benefits for breastfeeding. Breast milk has antibodies that are transported to the baby and help them build their immune system and protect against diseases. Breast milk is also A wonderful source of diet. When a woman is breast -feeding, they may experience amenorrhea (when you do not have a monthly menstrual period). Breastfeeding may be a temporary form of birth control if the person is breastfeeding exclusively (ie, without formula), they have not yet had a menstrual period and the baby is less than 6 months. This method is sometimes called “LAM). LAM does not work for everyone and may not be reliable enough for all couples. Some people do not develop amenorrhea when breastfeeding, so another form of birth control will be recommended.
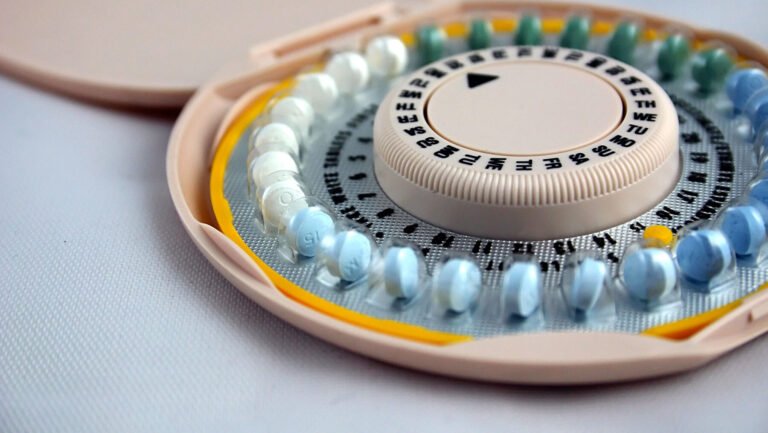
Are there any other forms of birth control I can use when breastfeeding?
Many contraceptive methods do not affect your breastfeeding. However, estrogen -containing options may reduce milk supply. Depending on the option you choose, your health care team may suggest wait up to 4-6 weeks After delivery, so that the supply of milk is well established and your body has recovered from childbirth.
Another factor is how serious you are to prevent another pregnancy. Some options such as IUD, hormonal implant and Depo-Prover injection are 98-99% effective in prevention of pregnancy (this means that only 1 or 2 of 100 women will become pregnant each year using these methods). Birth control pill is about 93% effective in prevention of pregnancy (this means that about 7 of 100 women will become pregnant each year using birth control pills). The condom is about 85% effective, depending on how carefully it is used (this means that about 15 of 100 women will become pregnant each year using this method).
The American College of Obstetricians and Gynecologists (ACOG) has a website answering frequently questions about contraceptives, including the advantages and disadvantages of each type: https://www.acog.org/womens-health/faqs/postpartum-birtrol
Hormonal birth control options
There are many types of hormonal birth control options, including oral pills (orally), injections, implants and some IUDs. Some options contain forms of both estrogen and progesterone, while some contain mere progesterone. In general, it is expected that only small quantities of hormones will pass to your mother marriage and these low levels are unlikely to lead to any side effects on your baby. However, some of them may affect milk supply.
Some estrogen -containing options include “combination birth control pills”, skin and vaginal ring. One disadvantage of estrogen is that it can reduce or even stop the supply of milk. Health-care providers usually recommend waiting to start estrogen-meters up to at least 4 weeks after delivery to allow milk to be well established.
Options only for progesterone include only Progestin pills (“mini pills”), injection (eg Depoproverta Shot), implant (eg nexplanon), hormonal intrauterine device (IUD) and emergency contraception. Only progesterone options generally Do not reduce the supply of milk or affect the quality of the milk. Some professional groups suggest waiting 4-6 weeks After birth before taking the depo-proverra shot because the amount of hormone In your blood and milk from this injection is higher around the time given.
Non -hormonal birth control options
Non -hormonal birth control options include barrier methods such as male and female condoms, sperm, diaphragms, cervical lid, sponge and IUD copper. None of these strategies affect the milk supply.
Methods
Other birth control options that do not include hormones or barrier elements are the diary tracking option and abstinence. The calendar tracking option is when you keep track of your menstrual cycle and avoid sexual intercourse on the days you are more fertile (most likely to become pregnant). This method is not very reliable After childbirth, because an menstrual cycle can be irregular in the first months. Abstinence is the avoidance of vaginal intercourse and the choice to be familiar with other ways that cannot lead to pregnancy. Abstinence is 100% effective in prevention of pregnancy.
Summary
In summary, what is the best birth control option during breastfeeding? Each person will be different, so it is important to talk to the healthcare provider about the choice that is best for you based on your timetable, efficiency, family planning decisions and other personal health factors.
Resources
2023. Birth control after childbirth. Frequently questions. American College of Obstetrics and Gynecology. https://www.acog.org/womens-health/faqs/postpartum-birth-control
Berens P, Labbok M? Academy of breastfeeding. ABM Clinical Protocol #13: Breastfeeding contraception, revised 2015. 2015 Jan-Feb, 10 (1): 3-12. DOI: 10.1089/bfm.2015.9999. PMID: 25551519.
2024. Contraception and methods of birth control. Disease Control and Prevention Centers. https://www.cdc.gov/contracepion/about/index.html
2024. About breastfeeding. Disease Control and Prevention Centers. https://www.cdc.gov/breastfeeding/php/about/index.html
Goulding Alison N., Wouk Kathryn, and Stuebe Alison M., contraception and breastfeeding in 4 months after childbirth among women who intend to breastfeed. Mammal medicine. January 2018, 13 (1): 75-80.
Stanton, Blumenthal Pd. Hormonal contraception after childbirth women. Curr Opin Obstet Gynecol. December 2019, 31 (6): 441-446. DOI: 10.1097/GCO.0000000000000571. PMID: 31436540.
Jessie poskochil, mgc, cgc He is a license and certified genetic adviser at the University of Nebraska Medical Center (UNMC) and works with her mother Nebraska. He specializes to see patients in the oncological environment for patients in Nebraska and Iowa. Jessie won her undergraduate diploma in Biology from the University of Nebraska-Linkoln and her degree in UNMC genetic counseling. It enjoys the teaching of today’s UNMC genetic advice students and is of particular interest to cancer treatment reports during pregnancy.