The research lays the foundation for the possibility that aggressive prostate cancer can potentially be detected through a few drops of semen or blood in the long term.
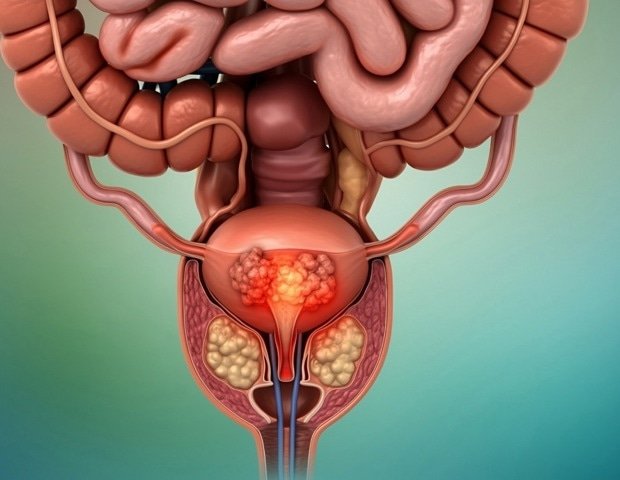
Prostate cancer is the most common form of cancer in men in Western countries.
Studies have found prostate cancer in half of men over 60 and about 70% of men over 80.
This shows that the disease is naturally associated with aging.
Prostate cancer often develops very slowly. For the vast majority, this is a disease that you live with well, without the need for treatment, but some have an aggressive variant with the cancer returning even after surgery. The disease behaves very differently from patient to patient. Understanding what makes cancer aggressive is crucial for better diagnosis and treatment.”
May-Britt Tessem, Professor, Norwegian University of Science and Technology (NTNU)
He believes existing methods are not good enough to detect who has a mild variant rather than those who have the aggressive type.
Aggressive cancer has its own genetic signature
Now, a research team from NTNU, led by Tessem, recently published an article in the highly regarded journal Nature Communications.
They are the first in the world to combine highly advanced research methods to detect aggressive prostate cancer.
In a large study, researchers analyzed prostate tissue using advanced methods combining genetic data, metabolic analyses, and detailed tissue imaging. The goal was to find new features that can predict which patients will develop aggressive disease.
They succeeded.
The results show two important findings.
Aggressive cancer has its own gene expression: The researchers identified a pattern in the gene expression of the tumor itself in prostate tissue in patients at high risk of recurrence and spread. This signature may become a new tool for distinguishing between patients who need intensive care and those who can manage with less intensive care.
Inflammation of apparently healthy tissue: Signs of inflammation and changes in metabolic processes were also found in normal tissue near the cancerous tumor. These glands had high activity of neurotransmitters that attract immune system cells and increased expression of a cell type that can trigger inflammatory reactions. At the same time, the levels of important substances had decreased, suggesting that the gland had lost its normal function.
“Aggressive prostate cancer appears to be associated with inflammation in the area around cancer cells, combined with specific genetic signatures and metabolic changes in prostate tissue. This knowledge may provide better methods for early identification of high-risk patients,” says Tessem.
The cancer comes back after surgery in 30 percent of patients
Prostate cancer progresses slowly, which means that research into this disease can be slow.
“It takes an average of nine years from surgery to recurrence. About 30 percent have cancer recurrence after surgical removal of the cancer. What we’ve done is to use samples from some patients who have relapsed and who we can thus define as having an aggressive disease and compare them with samples from those who had not relapsed and the patients who received active disease from ten patients. up to fifteen years ago, as a researcher, it’s important be persistent,” says Tessem.
The samples were taken in Trondheim and tested in patient groups of more than 2000 patients.
Today, prostate cancer is detected through a rectal exam by the doctor, and a blood test called PSA. Since it has become more common for men to have this blood test, the number of new cases of prostate cancer has skyrocketed. Now the number of new cases in Norway is about 5200 every year.
When more people are tested for a disease that occurs naturally as part of aging, doctors need to take the next medical step after the blood test to get a better clinical picture of the severity.
Today, this includes getting an MRI scan that provides a detailed picture of the prostate cancer gland and surrounding tissues.
It will reduce the threshold for easy control
Researcher Sebastian Krossa at NTNU was central to the research. He says it’s a known problem that many men are unaware of the disease and that the threshold for rectal examination is high.
“The PSA test obtained with a blood sample today is a correct and important step to lower this threshold. However, unfortunately it still requires resources to determine which patients need intensive follow-up. The goal of our research is to lay the foundations so that it is possible to easily check who has aggressive cancer, for example through blood or semen samples,” says Krossa.
Tessem emphasizes that preventing overtreatment is as important a goal as uncovering those who actually need treatment,
“We know that prostate treatment can significantly reduce quality of life with significant side effects for many patients, such as incontinence, erectile dysfunction and depression. Some patients require intensive treatment of the disease, but this is not always necessary. Many people are overtreated and suffer unnecessary discomfort as a result,” says Tessem.
Basic research, not ready for clinic
May-Britt Tessem and her team work with basic research, which means they study very basic and fundamental processes in the human body. This research has revealed entirely new characteristics and associations associated with cancer.
The new findings are an important piece of a larger puzzle that May they result in new and more practical discoveries in the future. Basic research is the most important source of important discoveries in medical treatment.
Tessem and her team used in situ multi-omic analysis technologies with a combination of transcriptomics, metabolomics and histopathology to map the tumor microenvironment in patients with aggressive prostate cancer.
Multi-omics technologies make it possible to obtain a 3D view of the tissue and what it is composed of. Tessem was awarded a prestigious European Research (ERC) Starting Grant for her research into prostate cancer.
Source:
Journal Reference: