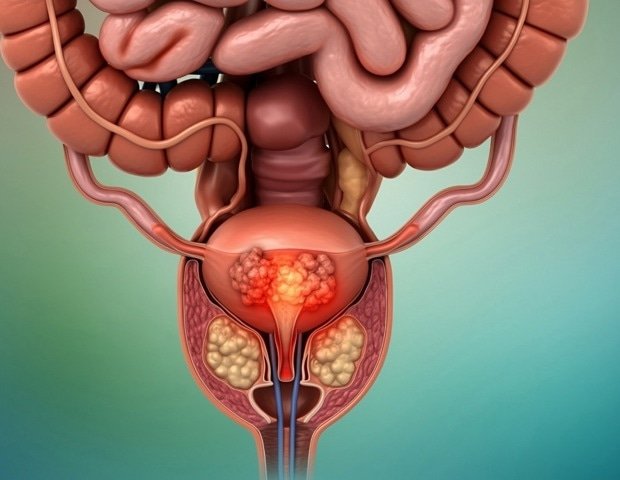
Researchers at the Cancer Center Johns Hopkins Kimmel, Johns Hopkins All Children’s Hospital and four other institutions have devised a new method to test prostate cancer using urine biomarkers, which are partially funded by the National Health Institutes. This approach could significantly reduce the need for invasive, often painful biopsies, they say.
By analyzing urine samples from patients with prostate cancer before and after prostate removal surgery, as well as healthy individuals, the researchers identified a group of three biomarkers – TTC3, H4C5 and EPCAM – which strongly detected the presence of prostate cancer. These biomarkers were detectable in patients before surgery, but were almost absent after surgery, confirming that they came from prostate tissue.
The researchers examined the table of three biomarkers in a development and ratification group. The test had an area below the curve (AUC) 0.92 (1.0 is a perfect performance). Accurately identified 91% of the time prostate cancer and accurately ruled out people without prostate cancer 84% of the time in the validation study. He also found that the table could be better than PCA3 to distinguish patients with prostate cancer than those with BPH.
The group maintained the diagnostic accuracy at 78.6% (development study) and 85.7% (validation study) of the Antigen Prostate (PSA)-prostate prostate and prostate cancer from benign prostate conditions with AUC 0.89. These results were published on September 2 at ebiomedicine.
TTC3 (Repeated Area 3) plays a role in asymmetric cell division into cancer cells, H4C5 (H4 aggregated tissue 5) plays a role in regulating chromatin structure (a DNA complex and protein found in cells) and EPCAM (EPCAM) on the surface of organs and structures throughout the body.
Prostate cancer, one of the main causes of death in men in the United States, is typically detected by blood tests to measure PSA, a protein produced by cancerous and non -cancerous tissue in the prostate. In most men, a level of PSA over 4.0 nanograms per milliliter is considered abnormal and can lead to a prostate biopsy composition, in which multiple tissue samples are collected through small needles.
However, the PSA test is not very specific, which means that prostate biopsies are often necessary to confirm the diagnosis of cancer, says senior author Ranjan Perera, Ph.D., Director of the Biology Center RNA in Johns Hopkins All Children’s Hospital Neurosurgery at Hopkins University. In many cases, these biopsies are negative and can lead to involuntary complications, Perera says. PSA tests can also lead to unnecessary treatment for a very low -grade prostate cancer that are very unlikely to grow and spread in a short period of time.
This new biomarker table offers a very promising, sensitive and special, non -invasive diagnostic test for prostate cancer. It is able to accurately detect prostate cancer, reduce unnecessary biopsies, improve diagnostic accuracy in patients with negative PSAs, and serve as a foundation for both laboratory and in vitro diagnostic tests. “
Ranjan Perera, Ph.D., Director of the RNA Biology Center in Johns Hopkins All Children’s Hospital in St. Petersburg, Florida and Professor of Oncology and Neurosurgery at Johns Hopkins University of Medicine
The panel was found to be able to detect prostate cancer even when the PSA was in the normal range and could distinguish prostate cancer from conditions such as prostatitis (prostate inflammation) and an expanded prostate, a condition known as the benign prostatic hyperplasia.
“There is a real need for biomarkers not based on PSA for prostate cancer and urine is quite easy to collect in the clinic,” says study by study Christian Pavlovich, MD, Bernard L. Schwartz distinguished Professor of Urological Oncology on Johns Hopkins of the Proto. “Most urologists believe that an accurate urine biomarker would be a valuable addition to our current diagnostic arsenal.”
During the study, researchers studied biomarkers in urine samples by healthy people as well as patients with biopsy prostate cancer underwent prostate surgery at Johns Hopkins Hospital, Johns Hopkins Bayview Medical Center for the celebration of Florida. They studied 341 urine samples (107 from healthy people, 136 from patients with prostate cancer prior to surgery and 98 after surgery) during urine testing and an additional 1,055 samples (162 from healthy persons, 484 by patients with prostate cancer and prostate cancer before surgery).
During the test phase of test performance, scientists also studied samples from BPH or prostatitis patients and healthy tests by Johns Hopkins Hospital from 2022-25.
Researchers exported RNA from prostate cells thrown into 50 ml urine samples and analyzed them using RNA sequence and also a quantitative chain chain in real -time polymerase (QPCR) to study gene expression. They also used immunocommunications to study biomarkers in samples of prostate cancer tissue and healthy neighboring tissue and statistical analyzes to compare biomarkers found in urine and tissue samples.
Of the original 815 genes specifically for the prostate identified by men with prostate cancer, the researchers prioritized the top 50 genes, then the top nine and from there they chose the three top performers: TTC3, H4C5 and EPCAM for further analysis.
Overall, the levels of expression of the three biomarkers were significantly higher in urine samples than people with prostate cancer than urine than healthy tests. The expression of each biomarker was reduced to low or undetectable levels in samples taken after surgery. A larger percentage of patients with prostate cancer has been positively tested for the three biomarkers than for PCA3, another biological marker associated with prostate cancers, both in the development study and in validation study.
“This test has the ability to help doctors improve the diagnostic accuracy of prostate cancer, reducing unnecessary interventions, while allowing timely treatment for those who need it,” says the co-author of the study Vipul Patel, MD, director of the Urological Oncology. Patel is also a medical director of Global Robotics for the Global Robotics Institute of Adventhealth and founder of the International Prostate Cancer Foundation. “On behalf of doctors and patients worldwide, I support further study and progress for these biomarkers.”
Researchers look at how the biomarker board could be used on its own or in combination with a PSA test to make a “super psa”, Perera says. The next steps for research are to conduct an independent test test at another institution and further develop the test for laboratory use in clinical environments, he says. The researchers have filed a patent and Johns Hopkins Technology Ventures helps the team overcome a company.
The co-authors of the study were Menglang Yuan, Kandarp Joshi, Yohei Sanada, Bongyong Lee, Rudramani Pokhrel, Alexandra Miller, Ernest K. Amankwah, Ignacio Gonzalez-Gomez, Narmagadda, Ezra Baraban, Anant Jaiswal and Johnaban Cheteghdewaw. Additional co-authors were from Charles University in Prague. The University of Kansas. Orlando Health Medical Group Urology Winter Park in Orlando, Florida. and the Adventhealth Cancer Institute.
The project was supported by the International Cancer Foundation for the Prostate Cancer, the Johns Hopkins Kimmel Cancer Center (Nih Grant # P30CA006973), the Bankhead-Coley Cancer Research Program (Grant # 24B16) in Perera and the Maryland Initiative Initiative at Pavlovich and Perera.
BetteGowda is a consultant to Haystack Oncology, Privo Technologies and Bionaut Labs. Is co -founder of Orisdx and Belay Diagnostics