As the aging of the population increases, could the complement routine help fight muscles and bones? This new revision emphasizes which emerging options have a real promise and where science still needs to cover the difference.
Review: In addition to calcium and vitamin D: Exploration of creatine, β-hydroxy-B-methyl bobby, prebiotics and probiotics in osteosacropenia. Credit Picture: Evgeniy Lee / Shutterstock
In a recent revision article published in the magazine NutrientsResearchers investigated the efficacy of emerging nutritional supplements, including prebiotics, probiotics and creatine, in improving muscle and bone health in elderly people with osteosacropenia.
They concluded that new supplements have the potential to play an important role in nutritional interventions aimed at improving bone and muscle synthesis and enhancing physical function in elderly adults. However, further research is needed to determine their effectiveness and identify which populations are most benefited. The review also emphasizes that the factors that affect bile metabolism are an emerging area of interest within the ox ox.
Increasing burden of osteosarpopenia
Osteosyrakropenia is an increasing health concern between elderly adults, determined by the combined presence of osteoporosis (impaired bone structure and low bone density) and sarcopenia (age loss with age).
As the global elderly population is expected to reach 1.5 billion by 2050, the prevalence of osteosaropenia is likely to increase, making the urgent issue of public health.
Osteoporosis increases the risk of fractures, especially in older adults who are also more prone to falls. Sarcopenia contributes to the loss of muscle strength and physical function and today there is no approved drug for its treatment.
When these two conditions appear together, they enhance the adverse effects of the other, increasing the risks of death, fall and disability.
The biological mechanisms behind osteosacropenia are complex. Shared risk factors, such as reduced protein metabolism, hormonal changes, oxidative stress and chronic inflammation, contribute to the deterioration of both bones and muscles.
Evidence shows that bones and muscles communicate through biochemical signals, such as myocins (from muscles) and osteocins (from bones) and through mechanical interactions. Therefore, interventions aimed at one web can also benefit the other.
Typical management usually involves physical activity and adequate intake of calcium, vitamin D and protein. However, emerging research suggests that new supplements, such as Hydroxymethytic (HMB), creatine, probiotics, prebiotics and compounds that affect bile metabolism, can offer additional benefits.
These may include reducing inflammation, reducing the risk of falling and enhancing muscle mass and strength.
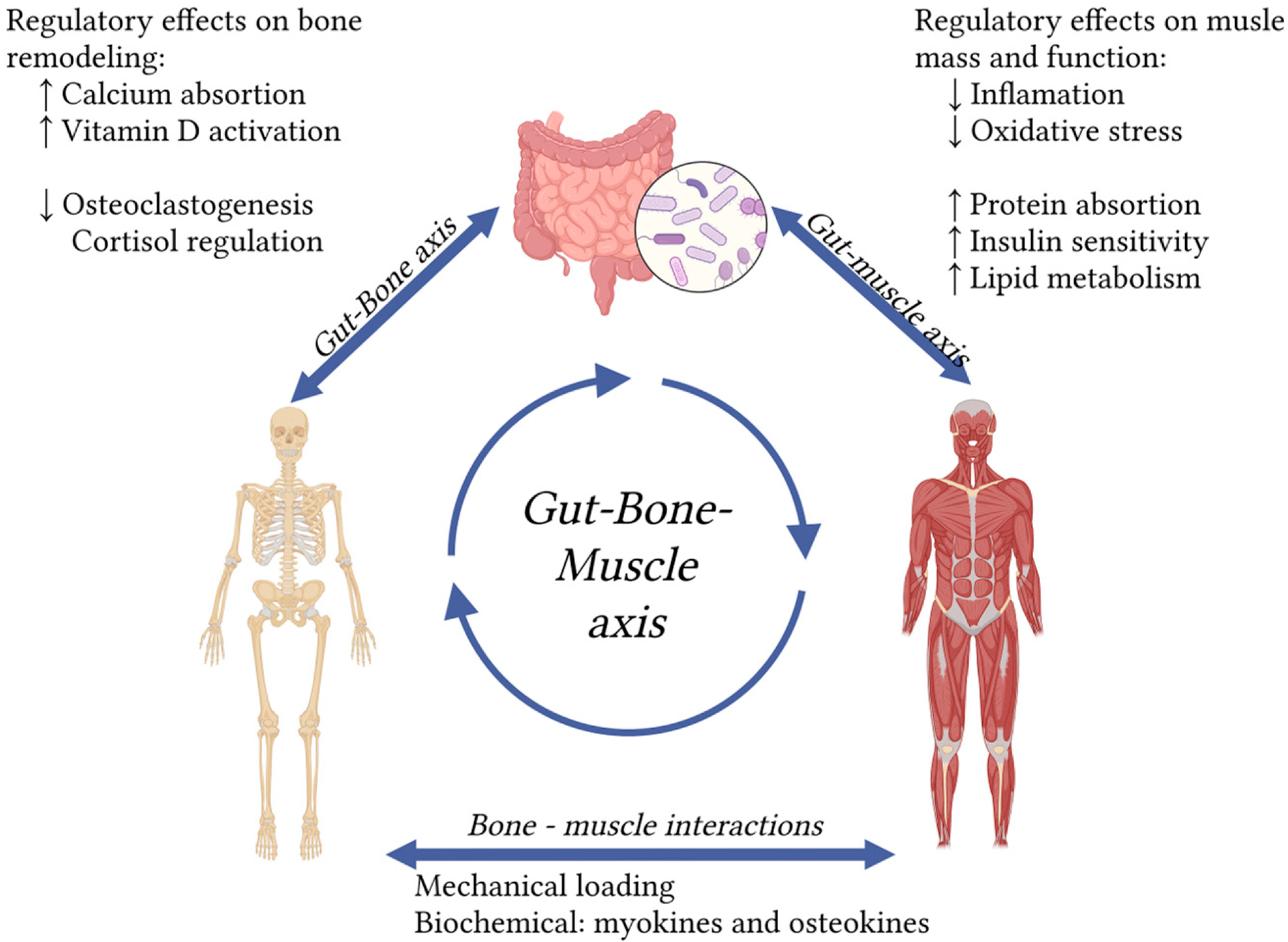 The axis of the bowl of the intestine emphasizes the effect of the intestinal germ on osteosacropenia. Arrows indicate interactions. ↑ indicates an increase. ❖ indicates a decrease. (created in https://biorender.com).
The axis of the bowl of the intestine emphasizes the effect of the intestinal germ on osteosacropenia. Arrows indicate interactions. ↑ indicates an increase. ❖ indicates a decrease. (created in https://biorender.com).
Creatine and osteosacropenia
Creatine is a vital compound for energy production, especially in muscles and brain. While the body produces some creatine, dietary sources, mainly fish and meat, are essential. The elderly often consume less creatine, making it complement a potentially beneficial choice.
Research shows that creatine, especially when combined with resistance training, enhances muscle mass, strength and function in older people, thereby reducing the risk of falling and improving mobility.
Creatine also supports bone health by enhancing the activity of osteoblasts and reducing bone split. However, recent studies do not indicate a significant increase in bone density in elderly adults. It can instead affect bone geometry and power indirectly through muscle profit.
The combination of creatine with protein, branched chain amino acids (BCAAS) or Vitamin D has been shown to provide additional muscle health benefits in some studies. However, there is currently no research on the synergy between creatine and prebiotics, probiotics or HMBs in elderly adults. The review specifically notes that combined complement studies (such as creatine plus HMB or creatine plus probiotics) have not been carried out in older populations.
The role of HMB in muscle and bone loss associated with age
HMB, a metabolite of Lefkini amino acids, has gained interest in the ability to support muscle health in elderly adults. It enhances the synthesis of muscle proteins and reduces breakdown, possibly helping to maintain muscle mass during periods of inactivity or disease.
Completing up to three grams a day is considered safe, but the research findings are mixed. Some studies have shown that HMB improves the power and muscle quality, especially with prolonged use of over 12 weeks. However, the effects on the mass of skeletal muscles and physical performance remain inconsistent, and most tests only prove only minor or non -significant effects on muscle mass.
Most elements are not available for older adults inhabited in the community. Few studies have been conducted and the results are moderate, with statistical significance observed mainly for handle force, instead of mass or efficiency.
The elements of the role of HMB in bone health are limited to animal studies, without randomized controlled tests in humans. HMB can work synergistically with other supplements, such as vitamin D, creatine, protein and probiotics, to enhance muscle and growth growth effects. However, the results vary depending on the combinations of population and complement. The review also notes the need for further research on the combined impact of HMB with other agents on older adults.
Prebiotics and probiotics aim at bone axis.
Prebiotics (unintentional fibers) and probiotics (living beneficial germs) can affect muscle and bone health by forming intestinal germ. Together, as synthetic, they enhance the microbial balance and promote anti -inflammatory effects.
Changes associated with aging in the gut are associated with sarcopenia and osteoporosis through mechanisms involving nutrient absorption, insulin sensitivity, inflammation and immune regulation.
The intestinal axis suggests that microbial strength and metabolism, while the axis of the oxen of the intestine has an impact on bone density through immunological configuration, hormone production and intestinal barrier.
Probiotics, such as Lactobacillus and Bifidobacterium, It can improve muscle function and mass. However, well -designed clinical trials in older adults are limited. The review clarifies that only one study in mildly fragile adults over 70 years of age showed improvement with L. Plantarum; Most elements for probiotic effects in the elderly are based on animal models or mixed populations. Similarly, some prebiotics have been shown to enhance bone health on animal models. Human data for older adults are rare and especially for the stem. Metabolites coming from the intestine also affect bone remodeling. Although mostly safe, probiotics can cause rare infections in vulnerable individuals, including bacteria or liver. Summary could improve the complexity of metabolites derived from the intestine, bile acids and roles within the intestinal-vibrant-tuch-axis, as analyzed in the review.
Conclusions
This review emphasized emerging nutritional supplements as promising strategies for managing osteosarpopenia in elderly adults.
These supplements are generally safe and well tolerated, with creatine showing the strongest elements for muscle improvement and indirect bone health support, especially when combined with exercise and other nutrients, such as protein and vitamin D.
HMB can enhance muscle strength, although the results are inconsistent. Probiotics and prebiotics offer potential through the configuration of the gut, but their results vary depending on the individual and bacterial strain.
Overall, these interventions show a promise, but further research is needed to optimize their use and identify the target populations.
