Español
One of the best tools your body has to stay healthy is your immune system. This elaborate, protective force inside you is designed to seek out and destroy hostile cells (things that don’t belong), such as viruses, bacteria, and sometimes cancer cells. However, cancer can be tricky because some cancer cells learn how to hide from the immune system so they are not recognized as a threat. When this happens, your immune system may not recognize them as an enemy and attack them as it should.
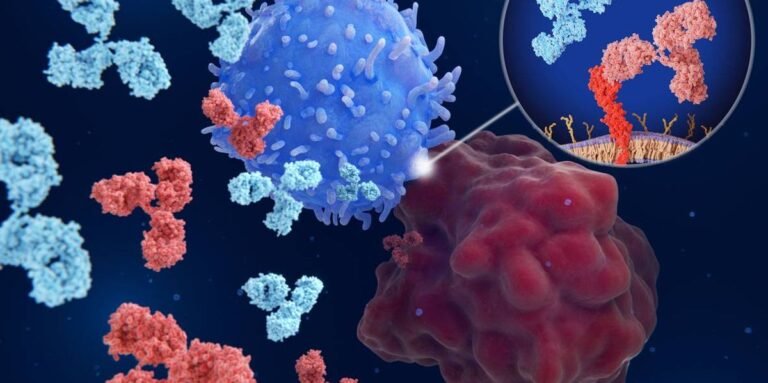
Immunotherapy is a type of treatment that helps your immune system work better against cancer. It boosts your immune system to help it find and attack the real threat. An important type of immunotherapy is called immune checkpoint inhibitors, which are drugs that help your immune system “see” cancer cells more clearly so it can attack them.
Here’s what you need to know about immune checkpoint inhibitors.
What is an immune checkpoint?
Your immune system is designed to attack things that don’t belong in your body. But, sometimes, when your immune system tries to target foreign cells, it has such a strong reaction that it kills healthy cells too.
Immune checkpoints are kind of like natural “brakes” that help control the immune system. They help turn the immune response on and off as needed so your body doesn’t accidentally attack itself.
How do immune checkpoint inhibitors work?
Immune checkpoint inhibitors help the immune system stay active so it can fight cancer cells more effectively.
Some cancer cells use special proteins to put the brakes on the immune system. When these proteins in the cancer cells bind to certain proteins in the immune cells, the immune system is turned off. This prevents the immune cells from attacking the cancer cells and allows the cancer to grow and spread.
Immune checkpoint inhibitors block this connection. When the “brakes” cannot be activated, the immune system remains alert and can attack the cancer cells.
Most immune checkpoint inhibitors are given as a liquid infusion through a vein. Some are given as an injection under the skin. A typical infusion session will last about 30 to 60 minutes, but you will likely need several infusion sessions during your treatment.
What are the different types of immune checkpoint inhibitors?
There are several types of immune checkpoint inhibitors. Each targets a different “off switch” in the immune system.
PD-1 and PD-L1 inhibitors: T cells, also called fighter cells, have a protein called PD-1 that helps them not attack healthy cells. Healthy cells have a corresponding protein called PD-L1. When PD-1 and PD-L1 bind, the immune response is turned off.
Some cancer cells also have PD-L1 proteins that trick the immune system into turning off, which allows the cancer cells to grow. PD-1 and PD-L1 inhibitors block this connection, preventing cancer cells from turning off the immune response so T cells can continue to fight cancer.
CTLA-4 inhibitors: Like PD-1, CTLA-4 is another protein on T cells that turns off the immune response, acting as an off switch for the immune system. CTLA-4 inhibitors block this switch, preventing the checkpoint from turning off so T cells can continue to fight cancer. This type of inhibitor is often used along with PD-1 and PD-L1 inhibitors for certain cancers.
LAG-3 inhibitors: LAG-3 is a checkpoint protein found in various types of immune cells, including T cells. It also acts as an off switch to prevent the immune system from attacking healthy cells. LAG-3 inhibitors prevent checkpoints from turning off the immune system so that immune cells can continue to attack cancer cells. Currently, this type of inhibitor (called relatlimab) is used with the PD-1 inhibitor called nivolumab to treat melanoma. Researchers are studying whether they can help treat other cancers as well.
What are the common side effects of immune checkpoint inhibitors?
Because immune checkpoint inhibitors activate the immune system, they can sometimes cause inflammation in almost any organ. These problems are called immune-related adverse events (irAEs).
They can range from mild problems – such as a rash or fever – to more serious problems, such as inflammation of the stomach and intestines or, in rare cases, the heart. Most side effects are mild, but serious, even life-threatening reactions can occur, so it’s important to report any new symptoms to your care team right away.
The most common side effects of an immune checkpoint inhibitor are rash, diarrhea, fatigue, and thyroid complications, but all kinds of side effects can result from inflammation. These side effects may include:
- Rash, itching, skin color changes — Skin toxicity (dermatitis)
- Coughing or difficulty breathing — inflammation of the lungs (pneumonitis)
- Chest pain — heart inflammation (myocarditis) or inflammation of the lining around the heart (pericarditis)
- Nausea, diarrhea or stomach pain — inflammation of the stomach or intestines (gastritis, colitis)
- Hepatitis — inflammation of the liver
- New diabetes — inflammation of the pancreas (pancreatitis) which can affect insulin production
- Thyroid problems — overactive or underactive thyroid (thyroiditis)
- Hypophysitis — inflammation of the pituitary gland, which can affect hormone levels
- Nephritis — inflammation of the kidneys
- Muscle weakness or numbness — inflammation of nerves or muscles (neuropathy or myositis)
How are immune checkpoint inhibitors used to treat cancer?
Since the first immune checkpoint inhibitor was approved in 2011, these drugs have become an important part of cancer treatment. Today, there are more than 100 approved uses for different checkpoint inhibitors. They are used to treat many types of cancer, including breast, lung, stomach, skin, kidney, and several blood cancers, among others.
These drugs were originally used mostly for metastatic cancer, meaning cancer that has spread to other parts of the body. Over time, research has shown that they can also help earlier in the course of the disease. Immune checkpoint inhibitors are now used to:
- Adjuvant setting — treatment given after surgery to reduce the chance of the cancer coming back
- Neoadjuvant treatment — treatment given before surgery to help shrink the tumor and improve outcomes
Whether your medical team recommends an immune checkpoint inhibitor depends on many factors, including the type of cancer you have, how advanced it is, what treatments you’ve already had, and your overall health.
Because these drugs activate the immune system, it is very important to pay attention to any new or changing symptoms during treatment. Treating side effects early helps your care team treat them quickly and prevent more serious problems.
Learning how to recognize these symptoms—and telling your care team right away—is a key part of staying safe while receiving immunotherapy.
This educational resource was created with the support ofm Merck.
From your website articles
Related articles around the web