From Dr. Erica
Health

Breast health is an incredibly important part of women’s (and men’s) health and wellness. Both women and men can develop breast disease, while men can even be diagnosed with breast cancer. Although this article will focus primarily on women’s breast health, anyone who is concerned about their breasts should contact their doctor for a thorough evaluation. A healthy breast includes several factors, such as size, shape and color. More importantly, regular screenings such as mammograms play an essential role in the early detection and prevention of breast cancer, a disease that affects millions of women every year.
What should healthy breasts look like?
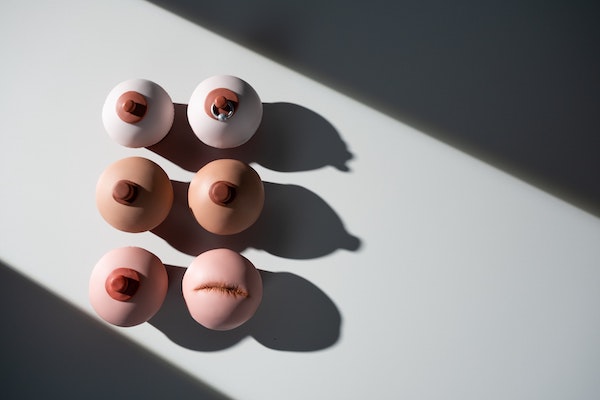
Breast size can vary greatly from person to person and what is considered healthy varies as well. There is no single definition of a healthy breast size. However, it is essential to understand that breast size alone is not an indicator of breast health. What is critical is that the breasts should be proportional to a person’s body and any sudden changes in size should be evaluated by a health professional. In addition, larger breasts can be more prone to certain discomforts such as back pain, so addressing these issues is essential for overall well-being.
Breast shape also varies quite a bit. Healthy breasts come in a variety of shapes, including round, drop, or asymmetrical. It is important to understand that breast asymmetry is common and rarely cause for concern. What is crucial is that any changes in the shape of the breast, such as dimpling, shrinkage, or unusual lumps, should be addressed immediately by a health care provider. Healthy breast color can vary from person to person, depending on factors such as skin tone and ethnicity. The key here is to be aware of any changes in breast or nipple color. Healthy breasts are usually a consistent color. Skin discoloration or thickening should be reported to a healthcare professional for evaluation.
Nipple discharge can be normal or medically concerning, so it’s always a good idea to report it to your doctor. Clear or light white discharge usually doesn’t indicate anything to worry about and can often be from healthy things like normal breastfeeding. However, women who are not breastfeeding may lactate (give milk from their nipples) and this may be a sign of a problem with their endocrine system, which requires medical evaluation. Yellow to green discharge can indicate infection, and bloody discharge can be from an injury or even cancer, so if you notice any drainage from your nipple, be sure to contact your doctor to schedule an evaluation.
Types of breast diseases
There are several types of breast disease, including benign (non-cancerous) and malignant (cancerous) conditions. Some common types are:
Fibroadenoma: A benign breast tumor composed of glandular and fibrous tissue. It is usually painless and feels like a smooth, firm lump.
Cysts: These are fluid-filled sacs that can develop in the breast tissue. They are often benign and can cause breast pain and tenderness, and may even become worse or more painful during your menstrual cycle.
Fibrocystic Change: Non-cancerous changes in breast tissue that can cause breast pain, lumps and discomfort.
Mastitis: Inflammation of breast tissue, often caused by infection or problems related to breastfeeding. Usually, this requires warm compresses and antibiotics are often prescribed.
It is important to note that while some breast diseases are benign, others can be malignant and potentially life-threatening. Regular breast self-exams, clinical breast exams, mammograms and other imaging techniques such as MRI and ultrasound are essential for early detection and appropriate management. If you have concerns about your breast health, consult a healthcare professional for evaluation and guidance.

Breast cancer
Besides skin cancer, breast cancer is the most common type of cancer found in women in the United States. The average risk of a woman in the US developing breast cancer in her lifetime is about 13%. The American Cancer Society estimates that in 2023, nearly 300,000 new cases of breast cancer will be diagnosed in the US. Breast cancer can present with many different signs and symptoms. Regular breast self-exams (such as knowing your ‘normal’ breast and seeking medical help with any changes), as well as preventive tests such as mammograms, are very important to catch cancer in its early stages, when it is easier to treat and before it spreads. in other areas of the body. Some of the more common signs/symptoms to look for include:
- New lump in the breast or armpit (usually painless, hard and/or irregularly shaped and not symmetrical).
- Change in breast size or shape (breast enlargement or a noticeable new change in one breast that grows in comparison to the other breast).
- Breast pain or tenderness (often, breast cancer is painless, but any new discomfort in your breast should be evaluated by a doctor to rule out an atypical manifestation of breast cancer).
- Changes in the skin (dimples, thickening, color change).
- Nipple changes (inversion when previously turned outward, redness/flaking, discharge, itching).
Despite its high incidence, advances in early diagnosis and treatment have led to a decrease in breast cancer mortality rates. Therefore, it is very important for women to understand the importance of breast screening and follow the recommended guidelines to increase the chances of early diagnosis and successful treatment. By staying informed, proactive, and vigilant about breast health, women can take meaningful steps toward hopefully reducing the impact of breast cancer on their lives and communities.

The importance of breast assessment
In addition to breast self-exams or in-office breast exams by your doctor, there are other methods available to evaluate breast disease, which include a variety of imaging tests.
A mammogram is a special type of X-ray that is used specifically on breast tissue for early detection of breast cancer. It is a diagnostic tool that can detect breast cancer at an early stage when treatment is most effective. Mammograms are usually performed by a radiologic technologist and interpreted by a radiologist. During a mammogram, your breast will be gently compressed between two flat plates, creating a clear image of the breast tissue. This compression may cause temporary discomfort, but it is necessary to obtain a high-quality image. The X-ray images are then analyzed for any abnormalities, such as tumors or calcifications.
There are two types of mammograms: preventive mammograms and diagnostic mammograms. Screening mammograms are usually done for asymptomatic women and are vital for early detection. Diagnostic mammograms are done when symptoms are present or when further evaluation is needed based on the results of a screening mammogram. Often, additional imaging, such as a breast ultrasound or breast MRI, will be ordered to follow up on an abnormal finding seen on the mammogram.
Breast MRI (also known as magnetic resonance imaging) is a medical imaging technique that uses magnets and radio waves to create detailed images of breast tissue. It often involves the use of a contrast dye injected into a vein. This contrast enhances the visibility of blood vessels and areas of increased blood flow, which is particularly useful for detecting tumors. A breast MRI can help detect breast cancers that may not be visible on mammograms or ultrasounds. It is often used in high-risk patients or when other imaging methods have inconclusive results.
A breast ultrasound, also called a breast ultrasound, uses high-frequency sound waves to create images of breast tissue. It is a non-invasive and radiation-free imaging method of breast imaging. It can help distinguish between fluid-filled cysts and solid masses, which may require additional imaging techniques to further evaluate the area in question. If a woman has particularly dense breasts, both mammography and ultrasound are often used to better visualize the breast tissue. Ultrasound may also be used if a breast needle biopsy is performed, because imaging can help with accurate needle placement.
Breast thermography is a technique that uses infrared technology to image variations in temperature and blood flow in breast tissue. It is based on the principle that cancer cells and other abnormal tissue may have increased blood flow and more metabolic activity, which may cause a slight increase in temperature compared to nearby healthy tissue. It has limited sensitivity and specificity, meaning it can lead to false positives and is therefore not a first-line or exclusively recommended imaging technique due to its low reliability.
The recommended frequency of breast imaging varies depending on several factors. Risk factors for breast cancer may include age over 50, family history of breast cancer, having certain gene mutations such as BRCA1 and BRCA2, dense breasts, early onset of menstruation or late menopause, alcohol use, obesity, radiation exposure and high hormone levels as seen in PCOS.
In general, women should start getting regular mammograms at age 40 and continue annually. However, women at higher risk of breast cancer may need to start screening earlier or have more frequent breast imaging. Sometimes, alternating between a mammogram and a breast MRI is even recommended. Since breast screening varies based on your personal and family history, developing a plan with your doctor is important to ensure proper screening and maintain your optimal health.