While mastectomy is often a necessary and proper therapeutic choice for many women with breast cancer, surgery can contribute to worst sexual health, body image and several other physical and emotional challenges after surgery, according to a new systematic review. Surgeons said the study emphasized the importance of women’s projection before undergoing mastectomy.
The research will be presented at the Clinical Conference of the American College of Surgeons (ACS) in Chicago, October 4-7.
As surgeons, we often focus on the medical side of care. There is no universal or standard approach to providing advice to women throughout the range of physical and emotional effects after mastectomy. As a result, many women get into surgery with an inadequate understanding of what to expect in the long run, not only physically, but emotionally and psychologically, after undergoing mastectomy. “
Lauren Raymond-King, MD, head of research and surgical resident at Yale Medical School in New Haven, Connecticut
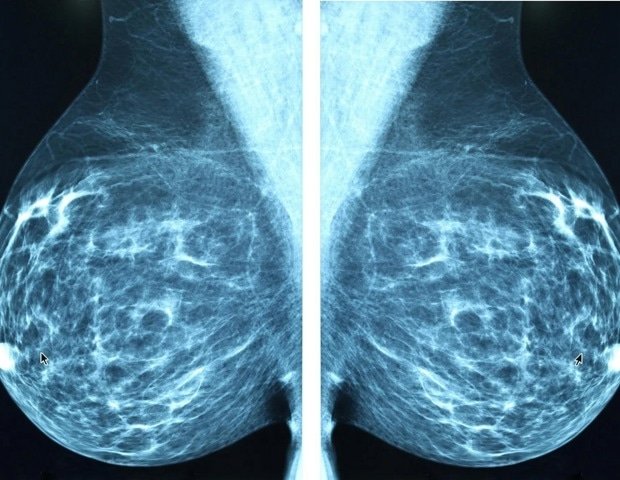
Although a common procedure, mastectomy, which involves removing one or both breasts, is an important surgery that requires long -term monitoring. More than a quarter of patients with breast cancer usually undergo mastectomy, and many patients remain in the hospital for shorter periods after surgery*- a tendency that has prompted researchers to analyze the results of patients after systematically.
From nearly 3,000 studies they identified, the researchers analyzed 20 studies that met their integration criteria, examining the effects of mastectomy on quality of life, sexual health and psychosocial well -being. All articles focused on the experience of women with breast cancer 1-3 stages. Studies involving women with stage 4 breast cancer, as well as women elected for prophylactic mastectomy to reduce the risk of cancer, were excluded from study due to separate needs and different overall medical decisions for these patients.
Basic findings
-
Worse psychosocial effects for women undergoing mastectomy: Fifteen of the 20 studies they analyzed reported worst psychosocial results, which measure the emotional, social and psychological effects of a disease for patients undergoing mastectomy in at least one psychosocial field.
-
There is no standard approach to evaluate post-surgery quality of life: There were 38 different outcome measures reported by the patient reported in all 20 studies. The most commonly estimated psychosocial areas were body image (55%), sexual health or sexual function (50%), pain or physical function (45%) and quality of life (40%). Much less estimated psychosocial health (35%) and satisfaction (25%).
-
Need for Standard Approach: Most output measures reported by the patient were used only once (72%), with studies ranging from the use of a dance of up to eight different PROMs to evaluate psychosocial effects after surgery. This great variant highlights the need to better prepare women with a validated viewing tool or other methods before undergoing mastectomy, the authors said.
“Breast cancer affects so many patients in our country and there is constant research to improve survival results,” said Elizabeth Berger, MD, MS, FACS, Senior Author of Research and Assistant Surgery Professor at Yale School of Medicine. “Now that there are many more survivors of breast cancer. We cannot miss the opportunity to study the effects of quality of life for our patients as they live so more after their diagnosis and treatment.”
The study is limited by the research included in the systematic review, which may differ from quality and study design, making it difficult to draw conclusions in all studies, the authors note. Future research will focus on the development of a validated projection tool designed to evaluate the readiness of women who face mastectomy.
Source:
Magazine report:
Raymond, L., et al. (2025) Systematic review of psychosocial effects between women with breast cancer undergoing mastectomy, scientific forum, clinical conference of the American College of Surgeons (ACS) 2025.