Three clinical trials led by researchers from The University of Texas MD Anderson Cancer Center have demonstrated significant positive results from new triple therapies in the treatment of relapsed or refractory and newly diagnosed leukemias. The results were presented at the American Society of Hematology (ASH) 66th Annual Meeting and Exposition. More information on all of MD Anderson’s ASH Annual Meeting content can be found at MDAnderson.org/ASH.
Study demonstrates robust overall responses with triple regimen including novel menin inhibitor (Abstract 216)
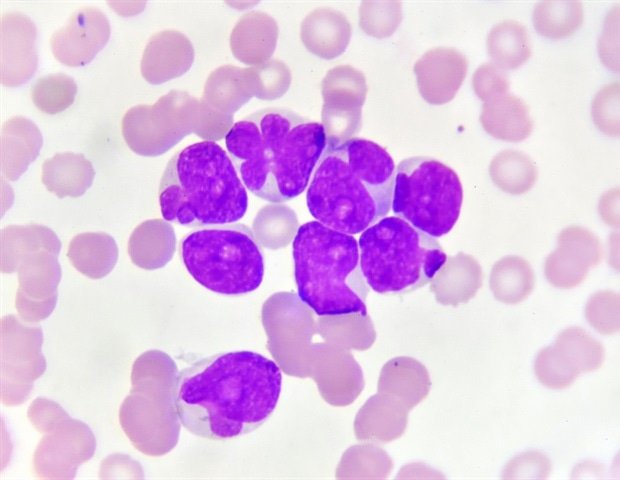
Combining the menin inhibitor, revumenib, with the hypomethylating agent, ASTX727, and venetoclax achieved an overall response rate of 82% in 33 adult and pediatric patients with relapsed or refractory advanced acute myeloid leukemia (AML) with KMT2A or NUP98ar results from the trial driving Phase I/II SAVE by Ghayas Issa, MD, associate professor of Leukemia.
Forty-eight percent of patients achieved complete remission or complete remission with partial hematologic recovery with these oral agents. Two patients completed maintenance therapy after receiving a stem cell transplant and remain in remission. The rate of measurable residual disease (MRD) negativity was lowest in patients with NUP98r rearrangements. With a median follow-up of 9.3 months, the six-month overall survival was 68% and the median duration of response was not reached.
We have demonstrated significant clinical benefits and efficacy from this treatment combination, which provides patients with an improved treatment option. This is an important step forward in the treatment of acute leukemia with these genetic rearrangements.”
Ghayas Issa, MD, Associate Professor of Leukemia
Revumenib is a potent, orally selective inhibitor of the menin-KMT2A interaction. In November, the Food and Drug Administration approved rebumenib as a single-agent therapy for the treatment of adult and pediatric patients with relapsed or refractory advanced acute leukemia with a KMT2A rearrangement based on results from Issa’s AUGMENT-101 clinical trial. To date, 33 patients have been enrolled in the SAVE trial, with a median age of 35 years. The trial also included five pediatric patients. Trial participants had an average of three prior lines of therapy. Of all patients, 16 had KMT2A rearrangements, 12 had NPM1 mutations, five had NUP98 rearrangements, and five had extramedullary disease.
Adverse events were manageable and consistent with previous studies. The most common side effects experienced by patients were prolongation of the QT interval on electrocardiogram monitoring and elevation of liver enzymes.
Issa presented updated findings December 7. The investigator-initiated trial is ongoing and continues to enroll patients. This study was supported by Astex and Syndax.
Triple therapy targeting IDH-1 mutant AML shows robust response with long-term follow-up (Abstract 219)
In a Phase Ib/II trial, the triple regimen of ivosidenib, venetoclax, and azacitidine showed an overall response rate of 94% and a composite complete remission rate of 93% in 56 patients with newly diagnosed or relapsed/refractory IDH1-mutated hematologic malignancies. including acute myeloid leukemia (AML), myelodysplastic syndromes and myeloproliferative neoplasms.
The trial was led by Courtney DiNardo, MD, professor of Leukemia, and presented by Jennifer Marvin-Peek, MD, clinical hematologist/oncologist.
The three-year overall survival rate was 70.5%, and patients who received a stem cell transplant had a three-year overall survival rate of 94.7%. Of trial participants who did not receive a stem cell transplant, 47% are still receiving trial treatment. Measurable residual disease negativity (MRD) by flow cytometry was achieved in 77% of patients. With a median follow-up of 36 months, median overall survival has not been reached at the time of data cut-off.
“This triple regimen is safe, well tolerated, and provided impressive response rates for those enrolled in the trial,” said Marvin-Peek. “So far, the results we’re seeing really position this triple regimen as a potential standard-of-care option for treating this subtype of AML.”
Previous research has identified ivosidenib in combination with azacitidine as an effective and well-tolerated treatment of IDH1-mutated AML. An additional clinical trial found venetoclax and azacitidine to be effective in treating this disease. Thus, researchers sought to explore triple combination therapy to further improve long-term patient outcomes.
The multicenter trial included 56 adult patients with newly diagnosed AML (31), relapsed/refractory AML (13), or myelodysplastic syndromes and myeloproliferative neoplasms (12). The median age of the participants was 69 years. Patients received an average of four cycles of treatment, although several patients received more than 40 cycles of the triple regimen.
Adverse events were consistent with those seen in previous studies with these drugs and were manageable with supportive care. The most common side effects were low blood counts and gastrointestinal side effects. Four patients also presented with differentiation syndrome.
Marvin-Peek presented updated findings on December 7. The trial was supported by both Servier and Abbvie/Genentech.
Triple first-line regimen for CLL yields high rates of undetectable measurable residual disease (Abstract 1011)
A triple regimen combining the non-covalent BTK inhibitor, pirtobrutinib, with the CD20 monoclonal antibody, obinutuzumab, and the BCL2 inhibitor, venetoclax, showed high rates of undetectable measurable residual disease (MRD) in patients with previously untreated leukemia (ALL). the results of the Phase II trial were presented by Nitin Jain, MD, professor of Leukemia.
After 13 cycles, the undetectable MRD rate was 98% in bone marrow and 100% in blood at a sensitivity of 10-4 – indicating less than one CLL cell per 10,000 lymphocytes – among 41 evaluable patients. The corresponding MRD rates at a more sensitive cutoff of 10-6 were 80% and 85% in bone marrow and blood, respectively.
“We are extremely impressed with the results of this first-line triple regimen for our patients, as we have seen some of the highest depths of remission we have ever seen in patients with CLL,” said Jain. “Today, we have several patients who are no longer on treatment and are being monitored with regular MRD blood tests.”
The trial involved 80 adult patients with an average age of 63 years. Of the trial participants, 79% had unmutated immunoglobulin heavy chain CLL and 13% had a del(17p)/TP53 mutation. As part of the trial, responses were monitored by imaging and bone marrow evaluation. MRD was assessed by next-generation sequencing in both blood and bone marrow after cycles 7 and 13. After completion of treatment, all patients are followed by blood MRD every three months for one year, followed by every six months.
The most common grade 3-4 adverse events were neutropenia and thrombocytopenia, which were consistent with previous trials.
Jain presented updated findings on December 9. The trial was funded by Eli Lilly.